Correlation of pre and immediate post-transplant factors with initial dd-cfDNA% in patients in a surveillance protocol
Guil Rozenbaum1,2, Andres Pelaez1,2, Juan C. Salgado1,2, Renata Ponsirenas4, Jeany P. Villamizar1,2, Sama Al-Bayati1,2, Mauricio Tellez1,2, Suresh Manickavel1,2, Mauricio Pipkin1,3, Juan C. Fernandez1,2.
1Miami Transplant Intitute, Jackson Health System, Miami, FL, United States; 2Division of Pulmonary and Critical Care, Miller School of Medicine Miami, University of Miami, Miami, FL, United States; 3Division of Thoracic Surgery and Lung Transplant, Miller School of Medicine Miami, University of Miami, Miami, FL, United States; 4Medical Affairs, CareDx, Inc, Brisbane, CA, United States
Introduction: Lung transplant has become a treatment option for many lung diseases. However, organ availability is limited. The first step for a successful lung transplant is donor selection based on the quality of the donor’s lungs, size matching, and geographic distance between the donor and recipient hospital. Donor-derived cell-free DNA (dd-cfDNA) is a noninvasive strategy for monitoring the health of allografts and is routinely used for surveillance after lung transplantation. It has been reported in kidney and heart transplantation that patients receiving DCD organs have higher levels of dd-cfDNA in the first months of the transplant. Here, we evaluate early post-transplant factors and their association with dd-cfDNA levels within the first months of transplant.
Methods: This was a retrospective analysis of all lung transplant recipients transplanted between March/2022 and July/2023. Multi-organ recipients were excluded from this analysis. Our surveillance protocol includes dd-cfDNA testing monthly post-discharge. We evaluated the differences in levels of first-drawn dd-cfDNA according to the following factors: length of stay post-transplant surgery, type of organ donation (DCD versus DBD), ischemia time, bilateral versus single transplants, patient age, biological sex and race, and recipient sensitization.
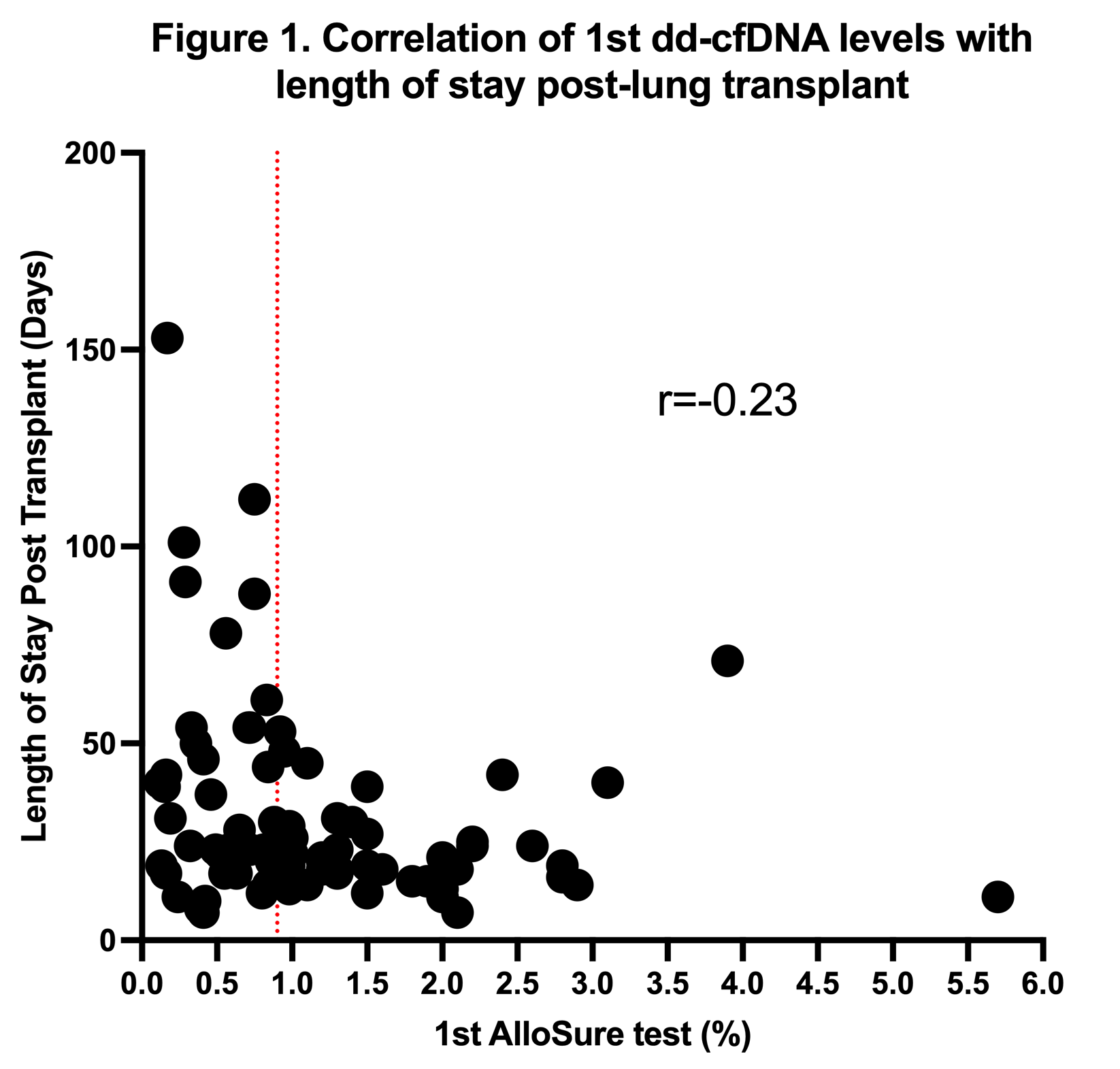
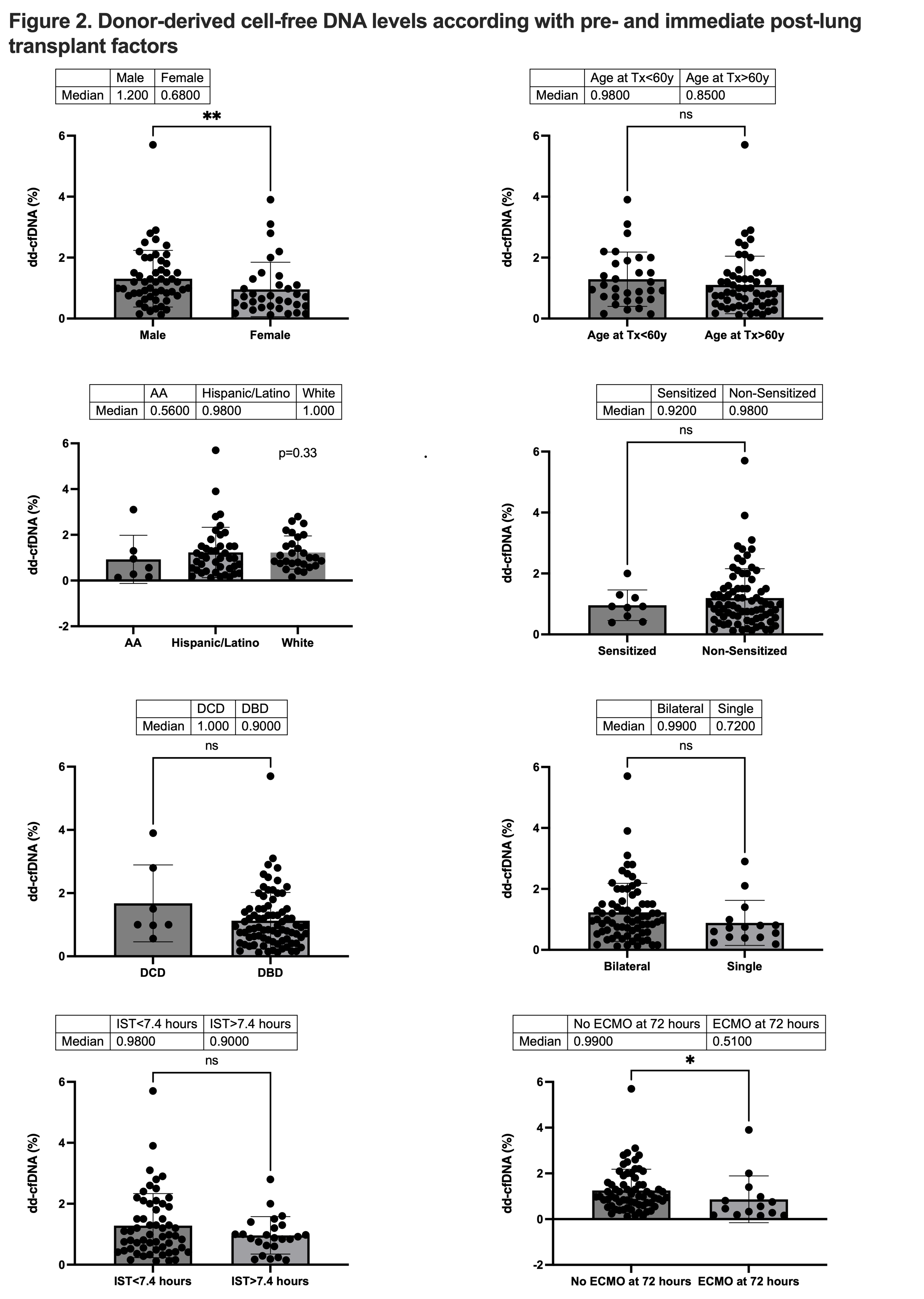
Results: Of the 119 lung transplant recipients transplanted during the studied period, 87 were included in this analysis. Five patients were excluded because they received another organ in addition to the LT, and 23 patients didn’t have dd-cfDNA draws in the first 3 months of transplant. Most patients were male (n=53, 60.9%), the mean age was 60.7 (10.9) years, 51.7% were Hispanic/Latino, and 39% were white. 7/87 patients received a DCD lung transplant, 82.8% (n=72) patients received a bilateral lung transplant, and 10% (n=9) patients were sensitized to HLA antibodies prior to transplantation. Average length of stay was 32.1 (±25.5) days, mean time to first dd-cfDNA draw was 45.95 (±27.5) days, and the median dd-cfDNA% for all population was 0.95%. There was no correlation between levels of dd-cfDNA and length of stay post-surgery (r=0.23) (Figure 1). Also, there were no statistical differences in levels of dd-cfDNA for the different characteristics, except for biological sex and need for ECMO in the first 72 hours (Figure 2).
Conclusion: Unlike other organ transplant data, our cohort didn’t indicate differences in dd-cfDNA levels between DCD and DBD lung recipients; this might be due to the small population of DCD recipients. The use of ECMO in the first 72 hours post-transplant was correlated with lower levels of dd-cfDNA, and male recipients showed higher levels of dd-cfDNA in our population. Understanding the factors that influence dd-cfDNA early post-transplant is essential to establishing a baseline for surveillance of future events.