Assessing European pancreas transplant practices to optimize patient outcomes
Hemant Sharma1, Omar Masood2, David Vandellen2, Zia Moinuddin2, Bence Forgacs2, Afshin Tavakoli2, Titus Augustine2, Raman Dhanda2.
1Transplant Surgery, Royal Liverpool University Hospital, Liverpool, United Kingdom; 2Transplant Surgery, Manchester Royal Infirmary, Manchester, United Kingdom
Purpose: Practice variability exists in pancreas transplantation, but the extent across the EU is unknown. We surveyed pancreas transplant surgeons to assess current practices.
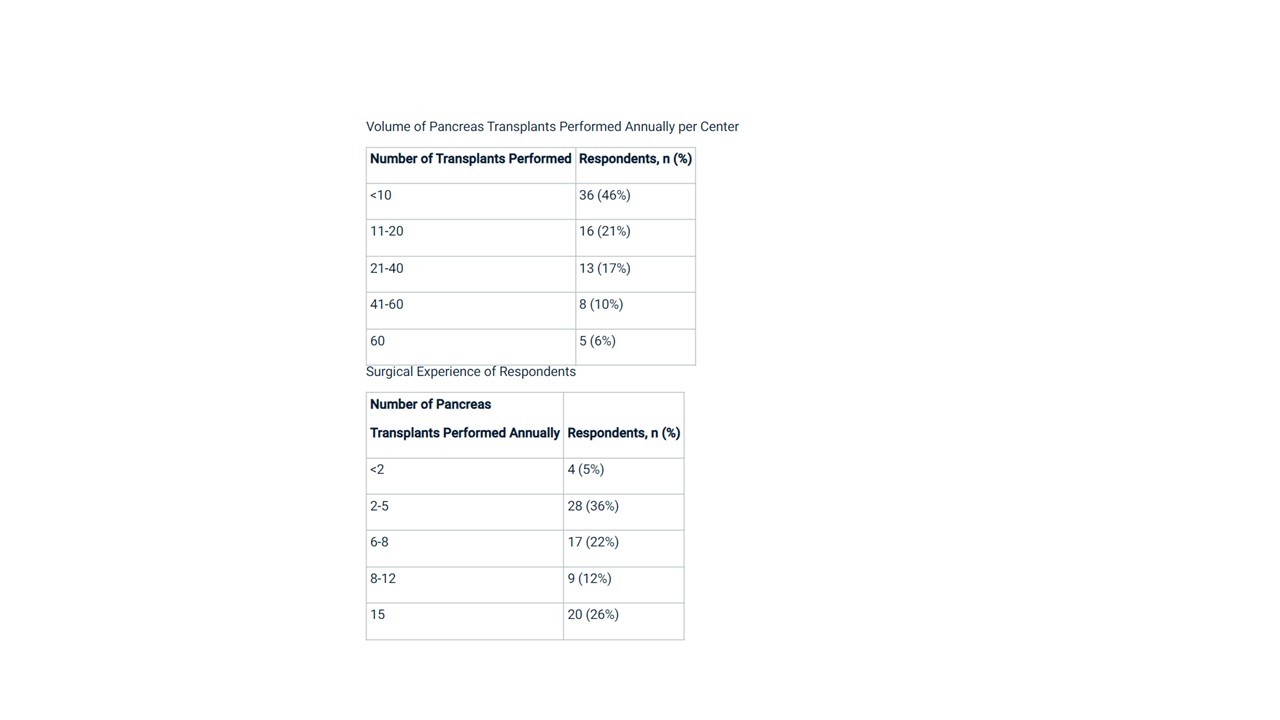
Methods: A 40-question survey was sent to 84 surgeons at 17 centres in 8 EU countries. Validity and reliability were analysed. Variability was evaluated using descriptive statistics and random effects modelling.
Results: The response rate was 92% (78/84). The survey demonstrated good validity and reliability (Cronbach’s alpha 0.82). Substantial variability existed in donor selection criteria such as acceptable BMI (range <10 to 35) and age (<30 to >60 years). Back-bench preparation also varied, including arterial reconstruction (52% continuous vs. 48% interrupted sutures) and duodenal closure (66% always buried staple line, 34% not). Systemic portal venous drainage was most common (70%), but 22% used portal drainage. Post-operative anticoagulation varied from 1 week to 3 months in duration. Random effects modelling found significant variability attributable to individual surgeons, centres, and case factors.
Conclusions: This rigorous survey identified modifiable targets to improve the quality and consistency of pancreas transplantation across the EU. Standardised best practice guidelines should focus on reducing variability in donor selection, back-bench preparation, surgical techniques, and post-operative management.