Fungal Fiasco! Unraveling graft pyelonephritis in early post renal transplant
Beauty Suman1, Himansu Sekhar Mahapatra1, Lalit Pursnani1, Muthukumar B1, Renju Binoy1, Tanvi Thakker1, Mahboob Alam1, Abhishek Jha1.
1Department of Nephrology , Atal Bihari Vajpayee Institute of Medical Sciences and Dr Ram Manohar Lohia Hospital , New Delhi , India
Background: Fungal infections are a rare but a significant complication following renal transplantation, posing a major threat to graft and patient survival. In India, the situation is further compounded by a unique epidemiological profile of high environmental fungal burden and poor socio-economic status.
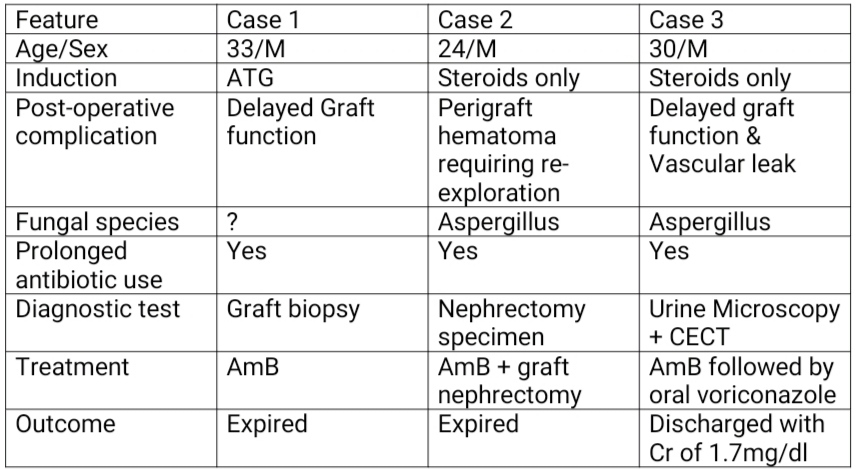
Aim of study: We report three cases of fungal graft pyelonephritis in allograft recipients, highlighting the clinical course, and treatment
Method: Case 1: 33-year old male with ESRD underwent renal transplant with mother as the donor with ATG induction. He developed allograft dysfunction on postop day 4.Urine culture revealed pseudomonas growth, and he was initiated on antibiotics. He developed lymphocele, leading to graft HDN and bladder compression. Deroofing surgery was performed. Persistent renal dysfunction prompted a graft biopsy, which confirmed fungal pyelonephritis. Am B therapy was subsequently commenced. A percutaneous nephrostomy was placed for persistent HDN, but there was no improvement in graft function. Patient ultimately succumbed to sepsis with shock. Case 2 - A 24-year old male with ESRD underwent renal transplant with father as donor with steroid induction. He was discharged at 3 weeks with creatinine levels of 0.8 mg/dL. DJ stent was removed at 5th week. Two days later, he developed high-grade fever, graft dysfunction, and pancytopenia. Urine culture grew pseudomonas. Despite antibiotics, fever persisted and antifungal therapy was initiated empirically. Graft nephrectomy was performed secondary to persistent sepsis with DIC. Graft specimen revealed invasive aspergillosis on histopathology. The patient did not improve despite therapy ultimately succumbing to septic shock. Case 3- 30 year old male, underwent renal transplant with brother as donor, with steroid induction. His urine output decreased on day 1 post op. Graft biopsy showed antibody mediated rejection and was started on plasmapheresis. On day 9, he developed a delayed vascular anastomotic leak for which he underwent re-exploration. Later his graft function started improving. 4 weeks after transplant he developed UTI with Klebsiella growth on urine culture. His DJ stent was removed and antibiotics were started and he improved. 6 weeks after transplant, he again developed fever with passage of fleshy material in urine. CECT KUB showed papillary necrosis. Because of persistent fever, he was empirically started on antibiotics and antifungals. His urinary debris showed fungal elements. He received Am B for 3 weeks and was discharged on oral antifungals with a creatinine of 1.7 mg/dl.
Conclusion: This case series highlights the severe adverse outcomes associated with early fungal graft pyelonephritis. A high index of suspicion should be present as early diagnosis and prompt antifungal therapy are crucial for improving patient outcomes. Even with graft nephrectomy and anti-fungal use, outcomes are dismal.
Department of Pathology, ABVIMS and Dr RML Hospital New Delhi . Department of Urology, ABVIMS and Dr RML Hospital New Delhi.
[1] ESRD End stage renal disease
[2] ATG Anti thymocyte Globulin
[3] Am B Amphotericin B
[4] DJ Stent Double J stent
[5] UTI Urinary tract infection
[6] HDN Hydronephrosis
[7] DIC Disseminated intravascular coagulation
