Correction of portal vein stenosis in patients following living donor liver transplantation
Konstantin Semash1,2, Timur Dzhanbekov1,2.
1General Surgery Department, National Children's Medical Center, Tashkent, Uzbekistan; 2Department of hepatio-biliary surgery and liver transplantation, V. Vakhidov Republican Specialized Scientific and Practical Medical Center of Surgery, Tashkent, Uzbekistan
Introduction: Anastomotic portal vein stricture occasionally occurs as a post-operative complication of a living-donor liver transplantation. Portal vein stenosis decreases portal venous blood supply to the liver graft and increases extrahepatic portal venous pressure, which may lead to liver dysfunction, splenomegaly, gastrointestinal bleeding, pancytopenia, intestinal edema, and ascites.
Methods: We treated 5 patients who came to our center from different clinics representing with clinical features of bilirubinemia and signs of portal hypertension (cytopenia, ascites) that occurred after liver transplantation. In all cases, portal vein stenosis was diagnosed by ultrasound and contrast enhanced computed tomography. The results of endovascular interventions on the portal vein were assessed.
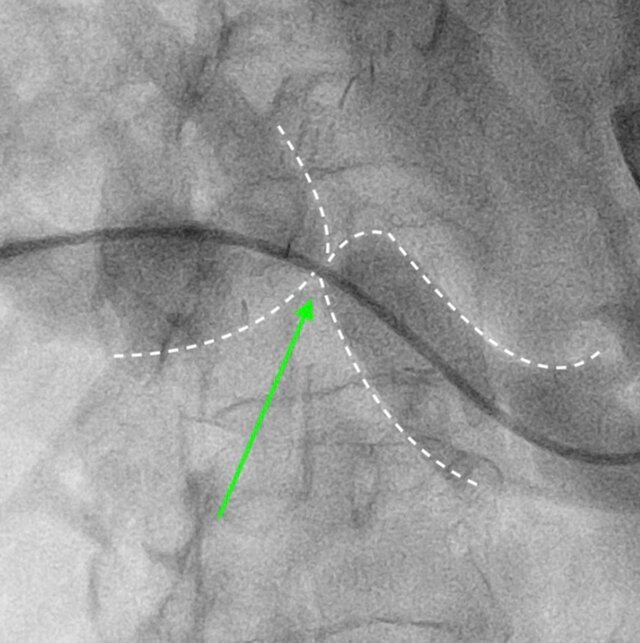
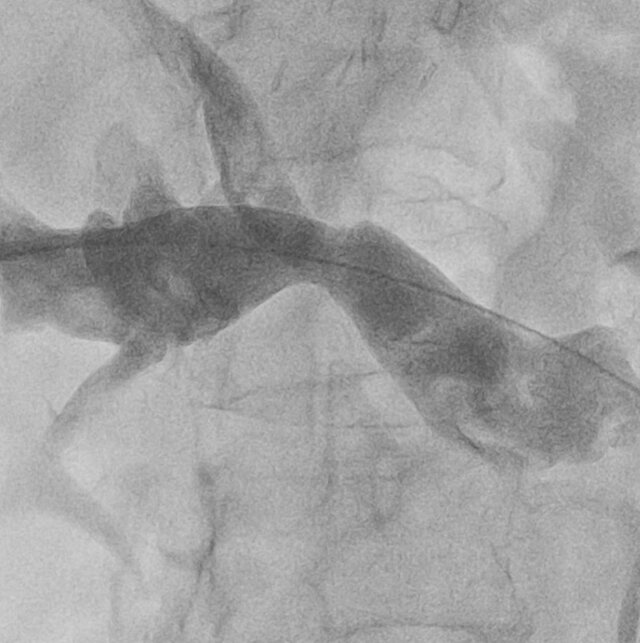
Results: All patients were treated using percutaneous transhepatic correction of portal vein stenosis with balloon plasty. In all cases ultrasound guided percutaneous approach to portal vein was performed. Balloon plasty was performed in all cases, no stents were used. No post operative complications occured. Signs of portal hypertension and graft dysfunction regressed after an average of one month of observation. There were no recurrences during 12 months of follow-up.
Conclusions: These cases highlight the importance of considering portal vein stenosis in the differential diagnosis of late-onset portal hypertension symptoms following liver transplantation. The optimal treatment method is endovascular intervetion.
[1] living donor liver transplantation
[2] portal vein stenosis
[3] portal hypertension
[4] endovascular intervention
