Living donor liver transplantation in biliary atresia with a portal vein less than two millimeters in diameter
Mehmet A. Haberal1, Emre Karakaya1, Sedat Yildirim1, Atilla Sezgin2, Adem Safak1, Nedim Cekmen3, Mehmet Coskun4, Fatih Boyvat4.
1Department of General Surgery, Division of Transplantation, Baskent University, Ankara, Turkey; 2Department of Cardiovascular Surgery, Baskent University, Ankara, Turkey; 3Department of Anaesthiology and Reanimation, Baskent University, Ankara, Turkey; 4Department of Radiology, Baskent University, Ankara, Turkey
Introduction: Biliary atresia is one of the leading indications for liver transplantation (LT) in children. In the pre-LT period in children, hemodynamic disturbances may occur due to portal vein (PV) hypoplasia caused by recurrent cholangitis. Among these cases, especially in LT’s from living donors, diameter mismatches between the recipient and donor PV cause technical difficulties during anastomosis. In cases like this, PV reconstruction is usually performed using vein graft. In our case report, we present a successful anastomosis between confluence of splenic vein-superior mesenteric vein and the donor PV without the use of a graft.
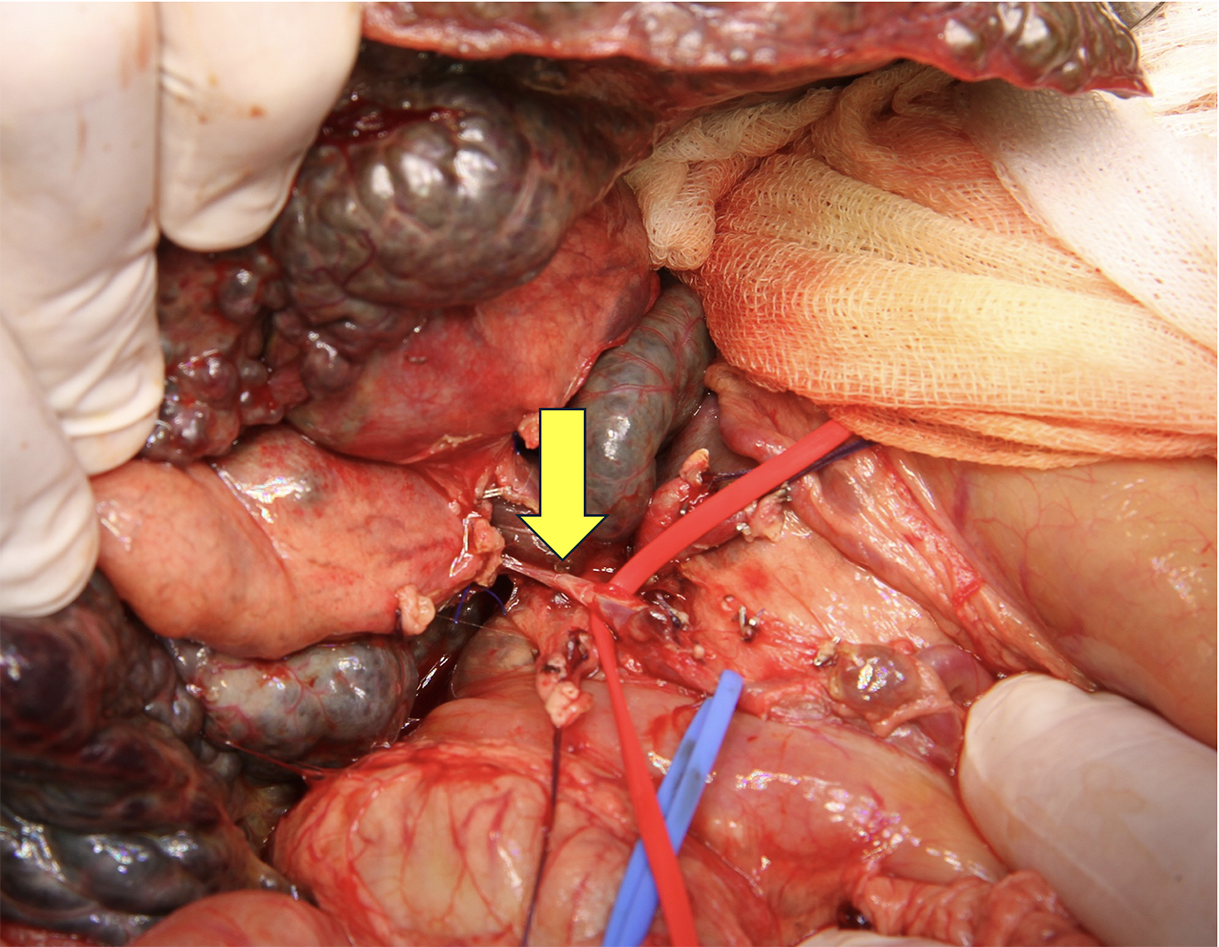
Material and Methods: Our case with biliary atresia was consulted to our center from Georgia. She was 18 months old and weighed 8 kilos. Her model for pediatric end-stage liver disease score was 22.2. Vascular structures were evaluated with preoperative CT angiography (CTA) and no flow could be seen in PV because it was completely occluded. Left lateral lobe living donor LT was performed by our experienced team from her father. In the recipient operation, hepatic vein anastomosis were performed using microvascular techniques. The hypoplasic PV was carefully dissected until the confluence of the recipient's superior mesenteric vein and splenic vein. Intraoperative measurement showed that the diameter of the portal vein was less than 2 mm (Figure 1). The graft portal vein was anastomosed to confluence with 6-0 polydioxanone absorbable monofilaments. The graft hepatic artery was then duct-to-duct anastomosed with the recipient's common hepatic artery. After confirmation of sufficient flow in all vascular structures by Doppler ultrasonography, biliary reconstruction was achieved using a Roux-en-Y hepaticojejunostomy. The LT was successfully completed. Intravenous heparin infusion was given as anticoagulant therapy for the first 1 week postoperatively and portal vein flow monitoring was performed twice a day with Doppler ultrasonography.
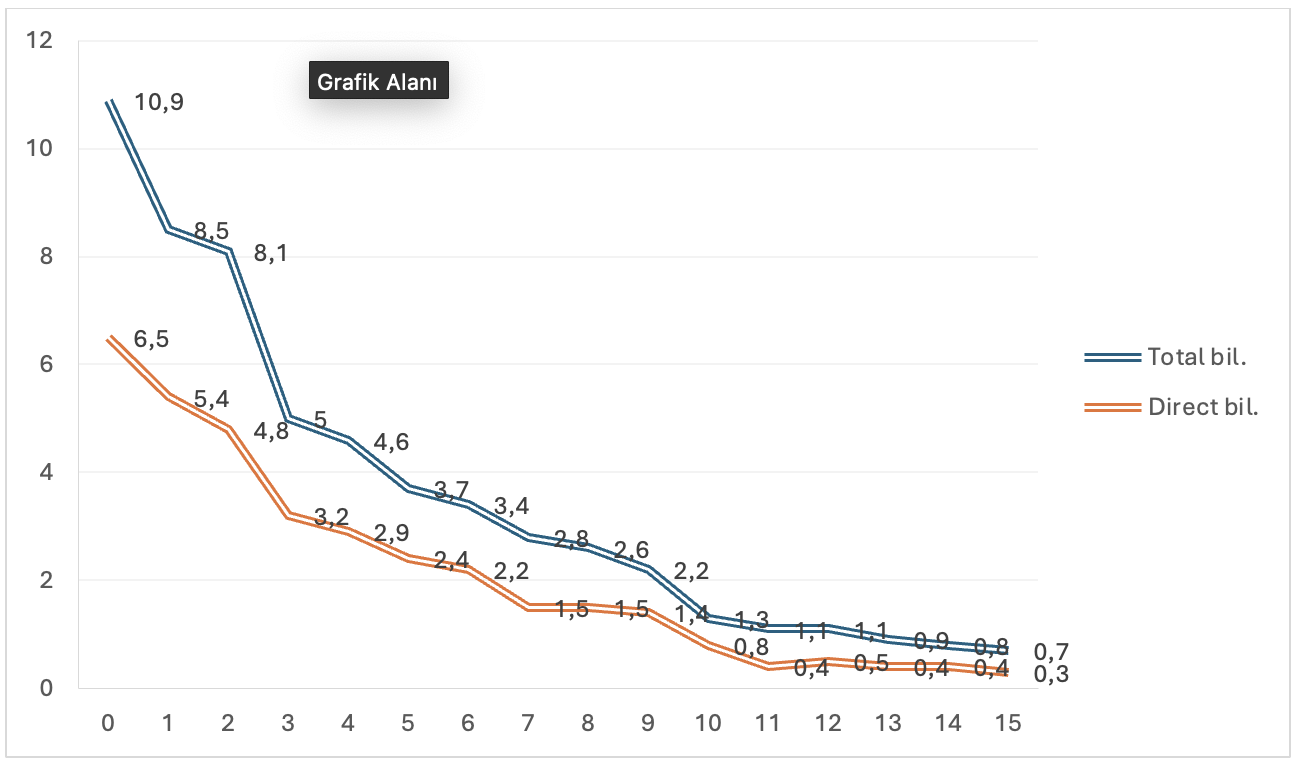
Result: Doppler ultrasonography on postoperative day 2 revealed stenosis in the portal vein. This stenosis was were successfully treated with a course of percutaneous transsplenic PV dilatation with a 3mm balloon and 6mm stent placement. In addition, because the patient had splenomegaly, steel syndrome was detected in hepatic artery flow. Coil embolization of the splenic artery was performed and sufficient flow in the hepatic artery was achieved. On postoperative day 14, AST value decreased from 1221 U/L to 50 U/L and ALT value decreased from 1179 U/L to 74 U/L. Total bilurubin value decreased from 12.8 mg/dl to 0.7 mg/dl and direct bilurubin value decreased from 9.1 mg/dl to 0.3 mg/dl (Figure-2).
Conclusion: In biliary atresia, when there is a diameter mismatch between the recipient and graft portal vein due to portal vein obstruction or stenosis, anastomosis can be successfully achived between the graft portal vein and of the distal portal vein including confluence in experienced transplantation centers.