Biliary complications incidence, risks and outcome after liver transplantation : Low volume single center experience
Jamilya Saparbay1,2, Zhanat Spatayev dr1, Abylaikhan Sharmenov1, Shokhan Aytbayev1, Assylmurat Zhumukov1, Asan Zhexembayev1.
1School of Medicine, Nazarbayev University, Astana, Kazakhstan; 2department of HBP and transplant surgery, National Research Oncology Center, Astana, Kazakhstan
Liver transplantation program started in National Research Medical Center (NROC), Astana, Kazakhstan in 2013. It took a decade to establish current surgical and post LTx methodology. Similar to majority transplant centers in the world , biliary complications (BCs) are the most common complications after liver transplantation in our case series. Since LTx program inception biliary complications were the most complicated for management and required multidisciplinary team and commonly recovery is quite extensive.
This retrospective study analyzed incidence of biliary complications after living/deceased liver transplantation, performed in NROC between 2013 and 2023. All data for analysis were retrieved from electronic records. This study was approved by local ethical committee, informed consent was received from all patients for data retrieval,analysis and publication.
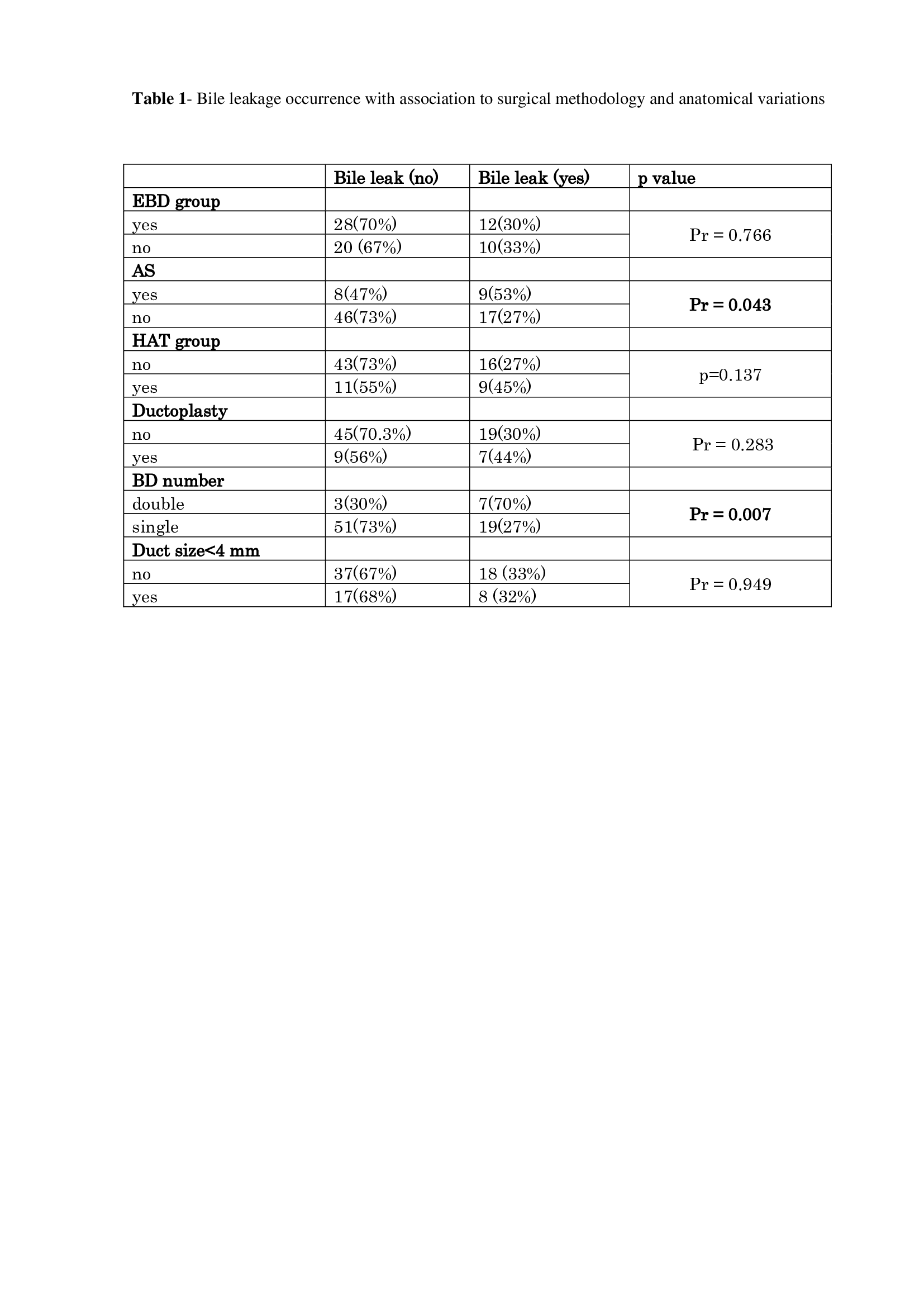
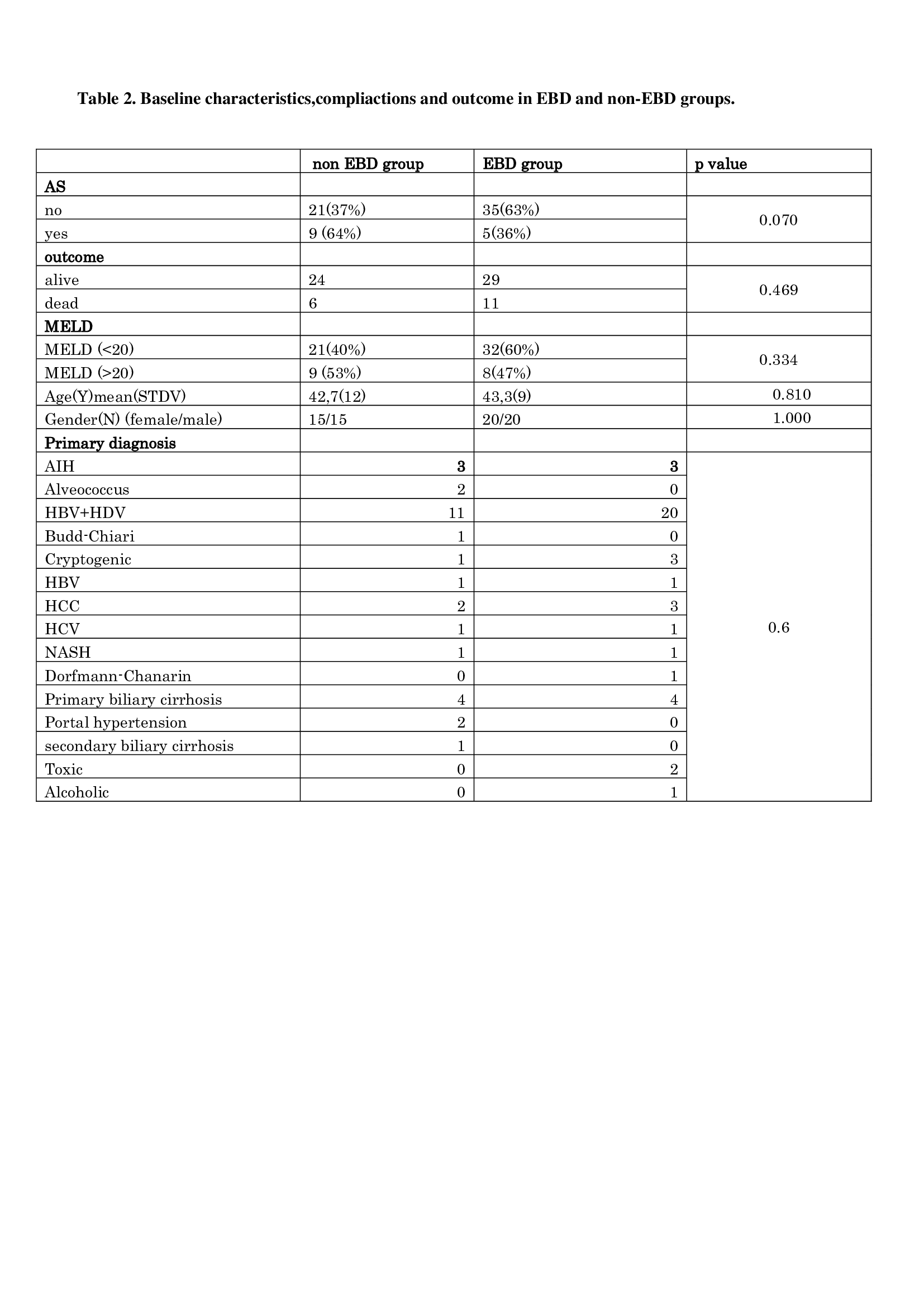
LTx from living donors were performed 61 cases (76.3%),in 19 cases (23.8%) liver grafts were received from deceased donors. Biliary tract reconstruction was performed with duct-to-duct anastomosis (DDA) in 64 cases(80%) and hepaticojejunostomy (HJ) in 16 cases (20%). A single DDA was performed in 70 patients; double DDA in 9 patients and triple DDA in 1 case. Bile duct diameter of harvested graft in 55 patients was more than 4 mm and less than 4 mm in 25 patients. Unification of multiple bile ducts was performed in 16 patients. Overall incidence of bile leakage in our study was 32,5%. Re-operation required in 3(3.8%)patients after bile leak was diagnosed. Anastomotic stricture occurred in 17 patients (21.2%). Hepatic artery complications, such as anastomotic thrombosis with consequent hepatic artery stenosis was detected in 20 patients (25,3%).Draining tube across biliary anastomosis(EBD) fixed with absorbable sutures and percutaneous placement on the skin was performed in 40(57,2%) recipients out of 70. Anastomotic stricture occurred more frequently in the group were bile leak developed after LTx and comprised 9 patients (53%),p value=0.043.Bile leakage incidence was significantly dependent on bile duct anastomosis number, bile leak happened in 19 patients, where single DDA was performed and in 7 cases were more than one DDA was done, p value-0.007.
Overall survival was analyzed in group with and without EBD group,1,3,5 year survival was 83% for all years and 73% in non-EBD and EBD group respectively, showing no statistical difference (p value-0.39). HAT occurrence was significantly associated with the death of the recipient, p value- 0.0000.
We found that BCs comprised the most frequent complication in our case series. Bile leakage was significantly associated with AS development, moreover AS occurred more frequently in EBD group. Limitation of our study included small patient number. However, placement of EBD appears to be a good choice for AS prevention.
[1] liver transplantation
[2] biliary complications
[3] external biliary drainage
