
Dr. Al Ammary is a transplant nephrologist, internist, and clinical researcher. He is an Associate Professor of Medicine at the University of California Irvine. He has formal graduate-level training in health services research (PhD). His specific areas of interest are (1) expanding the pool of living kidney donors across race/ethnicity and (2) advancing telemedicine services to enhance outreach and access to living donation and kidney transplantation. He is Chair of the Telemedicine Workgroup, American Society of Transplantation Living Donor Community of Practice.
Broadly, his work focuses on understanding and addressing the critical organ shortage of living donors in the United States. His studies have spanned a spectrum of topics related to my interests and with relevance to epidemiology, healthcare access and outcomes, and health policy.
The interplay of donor-recipient relationship and donor race in living liver donation in the United States
Fawaz Al Ammary1, Ahmet Gurakar2, Abhinav Humar3, Krista L Lentine5, Simeon Adeyemo1, Abdula Al-Seraji1, Suphamai Bunnapradist6, Alpesh N Amin1, Robert R Redfield III7, Abimereki D Muzaale2, Saleh A Alqahtani2,4.
1Medicine, University of California Irvine, Irvine, CA, United States; 2Medicine, Johns Hopkins University, Baltimore, MD, United States; 3Surgery, University of Pittsburgh, Pittsburgh, PA, United States; 4Medicine, King Faisal Specialist Hospital & Research Center, Riyadh, Saudi Arabia; 5Medicine, Saint Louis University, St. Louis, MO, United States; 6Medicine, University of California Los Angeles, Los Angeles, CA, United States; 7Surgery, University of California Irvine, Irvine, CA, United States
Living Donor Transplant Outcome Collaborative (LDTOC).
Background. Living liver donation improves survival of end-stage liver disease patients. Yet, it continues to represent a small proportion of U.S. liver transplantation with existing racial disparities. We investigated the interplay of donor-recipient relationship and donor race to better understand donor subgroups with no significant increase over the last decade.
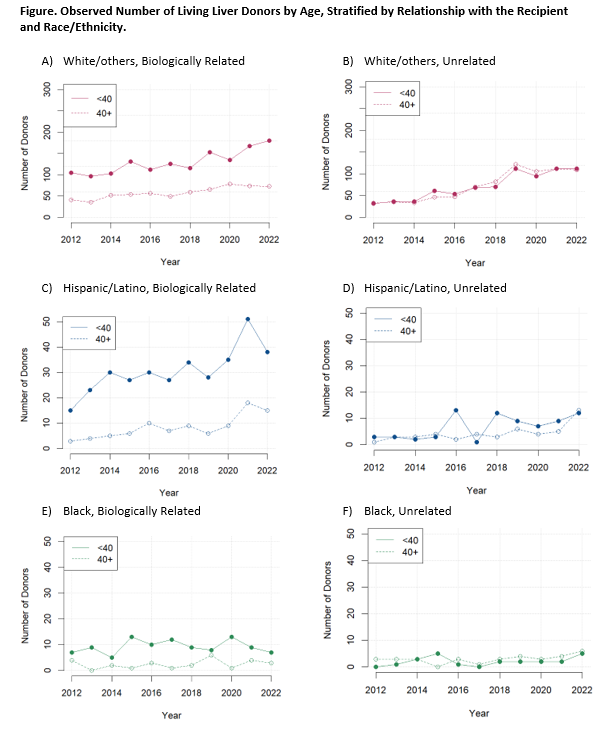
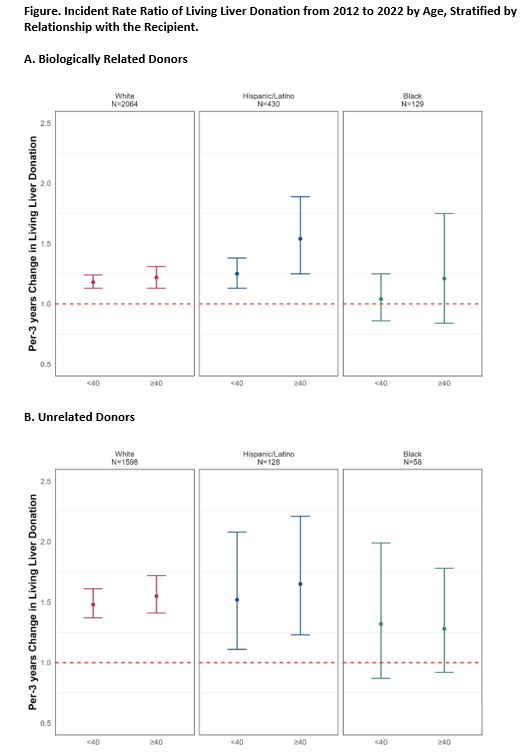
Methods. Using Scientific Registry of Transplant Recipients 1/1/2012-12/31/2022, we studied 4,407 living liver donors (median age=36 years; 83% were White, 13% Hispanic, 4% Black). We quantified the change in number of donors per 3-year increment (incidence rate ratio, IRR) using negative binomial regression, stratified by donor age, donor-recipient relationship, and race/ethnicity.
Results. From 2012 to 2022, the absolute number of biologically related donors increased from 175 to 316 (80% increase), and unrelated donors increased from 72 to 257 (257% increase). Among biologically related donors aged <40 and ≥40 years, White donors increased (IRR,1.131.181.24) and (IRR,1.131.221.31); Hispanic donors increased (IRR,1.131.251.38) and (IRR,1.251.541.89); and Black donors did not change. Similarly, among unrelated donors aged <40 and ≥40 years, White donors increased (IRR,1.371.481.61) and (IRR,1.411.551.72); Hispanic donors increased (IRR,1.111.522.08) and (IRR,1.231.652.21); and Black donors did not change. The observed trends of biologically related and unrelated donors were consistent across the U.S. transplant geographic regions, with substantial variations in the number of donors by region.
Conclusions. While biologically related donors make up the majority of donors, the number of unrelated donors has substantially risen in recent years primarily driven by White donors. Our findings highlight the opportunity to grow unrelated donors across race/ethnicity. Efforts are needed to understand modifiable barriers faced by Hispanic and Black individuals within family ties and communities and tailor culturally sensitive educational programs to motivate living donations.
The data reported here have been supplied by the Hennepin Healthcare Research Institute (HHRI) as the contractor for the Scientific Registry of Transplant Recipients (SRTR).
[1] Living donors
[2] Donor hepatectomy
[3] Liver transplant
[4] Race
[5] Registry
[6] Family
