
Clinical head of paediatric gastroenterology/hepatology at Charlotte Maxeke Johannesburg Academic Hospital, a tertiary academic hospital in Johannesburg, South Africa, since establishing the unit in 2015. She completed her speciality and subspeciality training at Red Cross Children’s Hospital in Cape Town in 2011. Her passion is paediatric liver transplantation, with her primary focus being to address disparities in transplantation and organ allocation and the impact of social determinants of health thus aiming to make the “gift of life” equally accessible to all South Africans. She also has a special interest in infectious diseases associated with liver transplantation and is a committee member of South African Transplant Society (SATS) and the Paediatric Committee in the ILTS and Interest Group (SIG): Infectious disease and transplantation and ALF SIG in the International Liver Transplant Society (ILTS). Her current role as the co-lead in the SATS liver working group is her current focus especially with a view to establishing a consensus regarding a workable liver transplantation allocation system in South Africa. She also belongs to IPTA and is a member of the IPTA outreach committee. She has published in international peer-reviewed journals and as first author on CMV in Paediatric liver transplantation in S.A and Prognostic markers in paediatric acute liver failure in S.A and is currently involved in numerous collaborative projects in paediatric transplantation.
Increased psychosocial risk factors in pediatric liver transplant patients transplanted for fulminant liver failure
Priya Walabh1,2,4, Anja Meyer3,4, Rachel Mlotha-Mitole1,2,4, Christina Hajinicolaou1,5.
1Paediatrics and Child Health, University of Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa; 2Paediatric gastroenterology, hepatology and nutrition, Charlotte Maxeke Johannesburg Academic Hospital, University of Witwatersrand, Johannesburg, South Africa; 3Transplant and Surgery, University of Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa; 4Gauteng Provincial Solid Organ Transplant Division, Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa; 5Paediatric gastroenterology, hepatology and nutrition, Chris Hani Baragwanath Hospital, University of Witwatersrand, Johannesburg, South Africa
Introduction: Acute (ALF) and chronic liver failure (CLF) in pediatric patients are two distinct conditions both in terms of etiology and outcomes in pediatric liver transplant recipients. In South Africa (S.A), Hepatitis A and other viral infections account for 60% of causes of ALF and biliary atresia (BA) for about 50% of CLF paediatric liver transplant (PLT) recipients. Psychosocial determinants greatly impact the outcomes of pediatric patients post liver transplant and can affect survival and quality of life. The aim of this study was to do a comparative analysis of outcomes (patient and graft survival) between ALF and CLF PLT recipients and to assess associated factors impacting outcomes.
Methods: Retrospective record review of all pediatric patients transplanted between 1 January 2013 till 31 December 2023 attending liver transplant clinic at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), a tertiary academic public/government sector hospital located in Johannesburg, South Africa. Permission to conduct the study was obtained from University of Witwatersrand HREC.
Results: Records of 104 PLT recipients were analyzed with median age at transplant of 34 months (19.5 – 84.15). There were 26/104 (25%) patients who were transplanted for ALF and 78/104 (75%) for CLF. Biliary atresia was the underlying cause for: 50/104 (48%) of children transplanted and hepatitis A virus accounted for acute liver failure in 10/104 (9.6%) of patients. There was no significant difference in outcomes between ALF and CLF patients. There was a significant difference in psychosocial risk factors between both groups {14/26 (54%) vs14/78(17.9%) P =0.001} with ALF patients having a significant increase in psychosocial risk factors which was also independently found to be a risk factor on multivariate analysis.
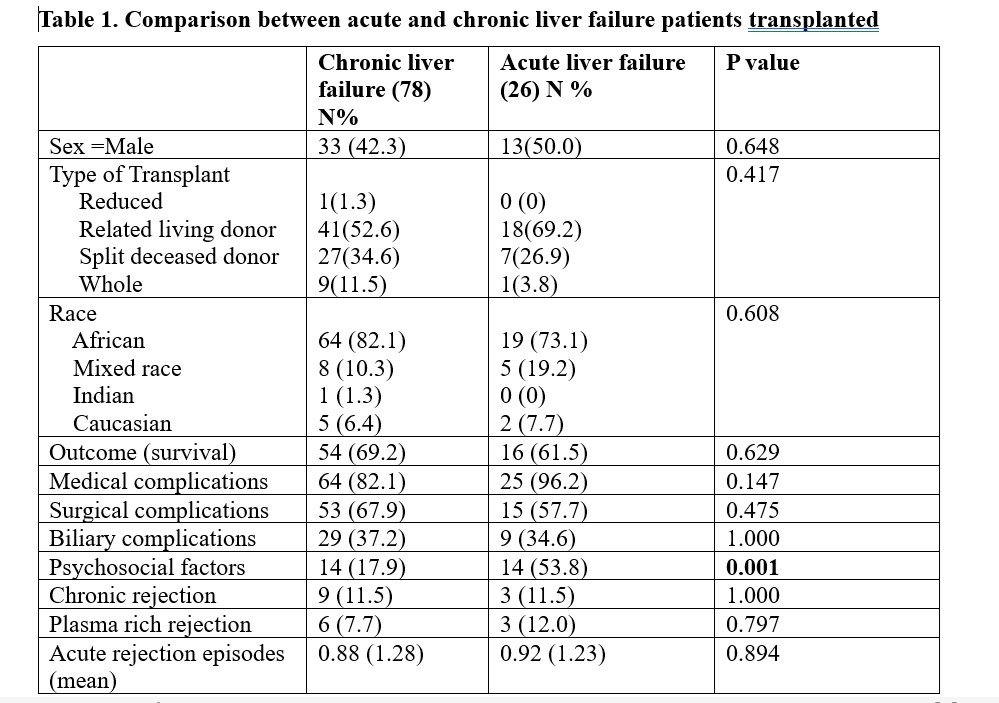
Conclusion: Psychosocial risk factors are independently associated with ALF compared to CLF in PLT recipients in a transplant centre in S.A. Despite this having no impact on patient and graft survival, psychosocial pretransplant criteria require further evaluation to better assess the ALF group of patients.
[1] fulminant liver failure
[2] psychosocial factors
[3] pediatric liver transplantation
[4] patient survival
[5] biliary complications
[6] medical complications
[7] allograft survival
[8] chronic liver failure
[9] viral infections
[10] hepatitis A
