Outcomes of pediatric Hepatocellular Carcinoma: A single-center experience with resection vs transplantation
Paula Medio Torrubiano1, Rosa Erro Aboytia3, Juan Cruz Abate 4, Claudia Palomo Martín1, Sofía Matesanz Zamarro1, Paula Ostos Santamaría1, María Margareto Sanabria1, Francisco Hernández Oliveros2,4, Ane Andrés Moreno2,4.
1Pediatric Surgery, University Autónoma de Madrid, Madrid, Spain; 2Pediatric Transplant Surgery, University Hospital La Paz, Madrid, Spain; 3Transplantation Department, Hospital Infantil de México Federico Gómez, Mexico City, Mexico; 4IdiPaz, University Hospital La Paz, Madrid, Spain
Background: Pediatric hepatocellular carcinoma (HCC) presents significant challenges due to its aggressive nature, with survival depending on complete resection. We aimed to assess outcomes between liver resection (LR) and liver transplantation (LT).
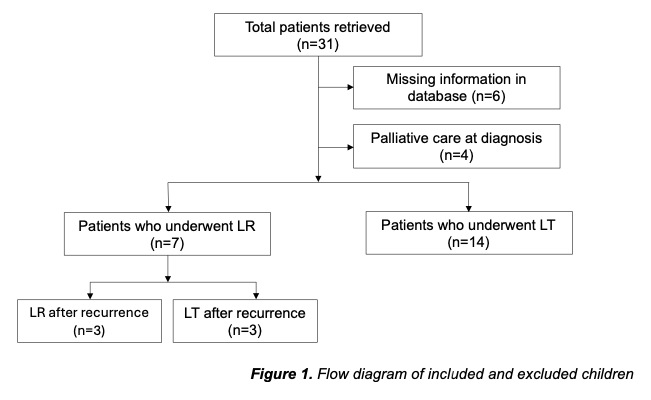
Methods: A total of 25 patients were retrieved, 4 of whom were classified as palliative at diagnosis. A subanalysis comparing cirrhotic liver (n=14) vs de novo (n=11) HCC was performed to identify confounding variables. Further evaluation focused on the 21 children with histologically confirmed HCC who underwent LR (n=7) vs LT (n=14). Kaplan-Meier survival curves were constructed.
Results: The mean age was 7.8 ± 6.1 years for patients with cirrhotic liver and 12.1 ± 3.5 years for de novo HCC. Our group observed overall total survival rates of 100%, 85% and 58% at 12, 36 and 60 months, respectively. De novo tumors had a higher recurrence rate and a poorer prognosis (P=.039 and P=.045). The disease-free survival at 60 months in our cohort was significantly lower among the LR group compared to the LT group (14% vs 82%; P=.0081). Recurrence after initial management (n=8) showed location differences between LR and LT. Preoperative alpha-fetoprotein (AFP) was elevated in 71% of children, but did not correlate with recurrence or compromised survival. Elevated AFP 3-months post-operation affected the course negatively (P=.044). Tumor number and diameter exhibited a trend towards poorer outcomes.
Conclusions: These findings emphasize the need for comprehensive pediatric surgical guidelines for HCC. We recommend LT over LR in pediatric cases. Extrahepatic disease post-neoadjuvant chemotherapy remains the only absolute contraindication.
[1] Pediatric hepatocellular carcinoma
[2] Surgical oncology
[3] Liver resection
[4] Liver transplantation
[5] Outcome
