Cytomegalovirus, aspergillus, influenza and xdr bacterial pneumoniae coinfection in kidney transplant patients: A case report
Cagla Sarikas1, Tuba Yanik1, Fatma Irem Yesiler2, Adem Safak3, Hande Arslan1, Mehmet A. Haberal3.
1Department of Infectious Disease and Clinical Microbiology, Baskent University, Ankara, Turkey; 2Department of Anesthesiology And Critical Care Unit , Baskent University, Ankara, Turkey; 3Department of General Surgery, Division of Transplantation, Baskent University, Ankara, Turkey
Introduction: CMV remains one of the serious infections complicating the course of organ transplant recipients particularly when causing coinfections by its immunmodulating property.Here we will present a renal recipient with CMV, Aspergillus, Influenza and XDR bacterial pneumoniae coinfections.
Case: A 52-year-old female patient, who underwent a renal transplantation from her father in 2015, was hospitalized in November, 2023 due to urinary tract infection, treated with Meropenem for 10 days. During this period, the patient received 1000 mg Prednisolone due to rejection episode.
1 month later, the patient admitted to the Dermatology department because of diffuse painful white plaques in the mouth, gingiva and palate. Upon detection of CMV PCR positivity intravenous ganciclovir (for 4 days) and valganciclovir ( for 24 days) were given.
On 12/01/24, during recieveing CMV treatment, the patient was admitted to ICU because of 2 week history of cough, dyspnea, and high flow oxygen require. Oseltamivir treatment was added to intravenous ganciclovir treatment because of Influenza PCR test positivity. Piperacillin tazobactam and Ciprofloxacin treatments were also given for suspected bacterial pneumonia.
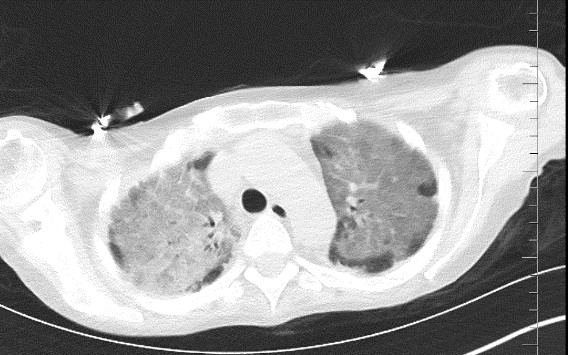
Serum galactomannan antigen test taken on the 2nd day of ICU hospitalization was found 0.65 S/CO but not was considered significant. Thorax CT scan performed on 18/01/24 revealed consolidation areas especially in the upper lobes and diffuse infiltration areas which were evaluated in favor of viral pneumonia in the foreground, and ARDS should be considered in the differential diagnosis (Figure 1).
On 22/01/24, fiberoptic bronchoscopy was performed, galactomannan antigen, CMV PCR and Influenza PCR tests were found positive in bronchoalveolar lavage. After fiberoptic bronchoscopy, the patient's condition worsened, she was intubated . Amphotericin B, Meropenem 2x1 gr and Colistin treatments were initiated upon XDR E.coli growth in the culture samples sent from bronchoalveolar lavage. Aspergillus niger growth was observed in fungal culture (Figure 2).
On the 15th day of intensive care unit hospitalization, the patient detoriated, ARDS progressed and died on 27/01/24.
Conclusion: Latent CMV infection is expected between 1 month to 1 year after transplantation and various CMV prevention strategies have been developed for this period. However, CMV latent infection can reactivate at any time after transplantation, particularly if immunosuppressive therapy is increased for any reason. Here we report a case of CMV disease with co-infections after rejection therapy. This case is an example showing that activation of cmv infection can develop not only in the first year after transplantation but at any time throughout life.

[1] CMV, Aspergilosis, Transplantation
