Are the recurrent glomerulonephritis (RGN) a negative factor for the long term renal transplant outcome?
Maria del Carmen Rial1, Luis R Leon1, Maria Fernanda Toniolo2, Olga E Guardia1, Francico Osella3, Javier Walther1.
1Renal Transplant Unit, Nephrology ITAC, Buenos Aires, Argentina; 2Renal Pathology, Nephrology ITAC, Buenos Aires, Argentina; 3Surgery Department, Nephrology ITAC, Buenos Aires, Argentina
The objective was to evaluate whether the patient and graft survival were worse when the diagnosis of kidney failure was RGN versus others causes.
RGN cases include: focal segmental glomerulosclerosis (FSGS) 70, IgA nephropathy (IgA) 59, membranoproliferative (MPGN) nephropathy 55, Lupus nephropathy (SLE) 45, Rapidly progressive glomerulonephritis (RPGN) 34, membranous 20, other 34.
Control group include: hypertensive nephropathy 88, polycystic disease (PKD) 76, uropathy 23, tubulointerstitial nephritis 19 and other 8. No diabetic patients were included.
T Student test and Chi square were used to group comparison. p value <0.05 was considered significant.
From a total of 2175 renal transplant performed since 1/1/2006 to 1/31/2022, 317 patients with histological diagnosis of RGN were transplanted with decease donor (214) or living donor (103). As control group, same number of patients matched by sex, age, type of donor and HLA compatibility were considered.
Most common immunosuppressive schema include Thymoglobuline as induction and mycophenolate+tacrolimus+steroids.
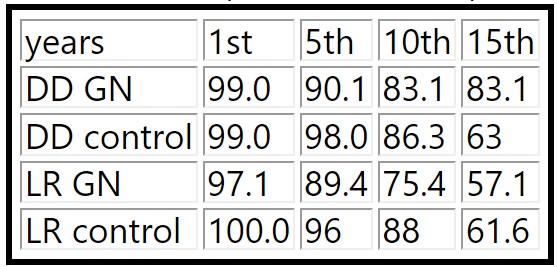
26 recurrences were observed during observational period: 9 FSGS, 6 MPGN, 4 IgA, 4 SLE, 3 membranous and 1 vasculitis. 8 were graft lost (4/9 FSGS, 2/6 MPGN, 1/4 IgA and 1/3 membranous). During post-transplant follow up protocol biopsies were not done unless clinically needed. No different rate of recurrence was observed according to donor type. Rejection rates were similar in both groups: 70/317 GN vs 68/317 control. Graft lost associated to rejection: 23/70 vs 15/68. Only FSGS showed marginal statistical trend to higher rejection. Patient and graft survival in both groups were not significantly different: (table 1 and 2)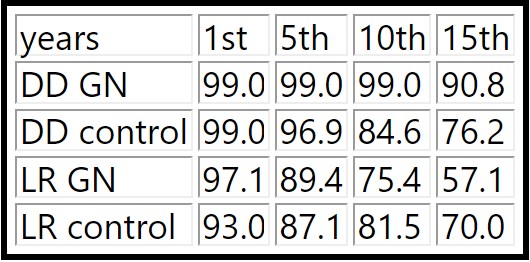
In our experience, GN primary disease was not identified as a risk factor of worse outcome regardless of donor type. The low incidence of recurrence could be explained by the lack of protocol biopsies. Low proportion of graft loss on patient with recurrence need more analysis.
