Atypical cervical cytology in solid organ transplantation patients: 20 years of experience in a single center
Nuri Alper Akbay2, Huseyin Akilli1, Tugba Tekelioglu1, Esra Kuscu1, Ali Haberal1, Ali Ayhan1, Mehmet A. Haberal3.
1Department of Gynecology and Obstetrics, Baskent University, Ankara, Turkey; 2Faculty of Medicine, Baskent University, Ankara, Turkey; 3Department of General Surgery, Division of Transplantation, Baskent University, Ankara, Turkey
Objective: Our aim was to discover the incidence and prognosis of atypical cervical lesions discovered in women who underwent a kidney or liver transplantation.
Methods: In this retrospective cohort study we’ve examined past medical records on Başkent Üniversitesi Ankara Hastanesi Electronic Health Records System and ultimately included 124 female patients who underwent cervical cytology screening tests following either a kidney or liver transplant in the years between 2003 and 2023.
Any patient who had records of biopsy and/or treatment results with no associated screening tests performed after the transplantation procedure were excluded from the study. Data analysis was done using the IBM SPSS Statistics (version 25) software.
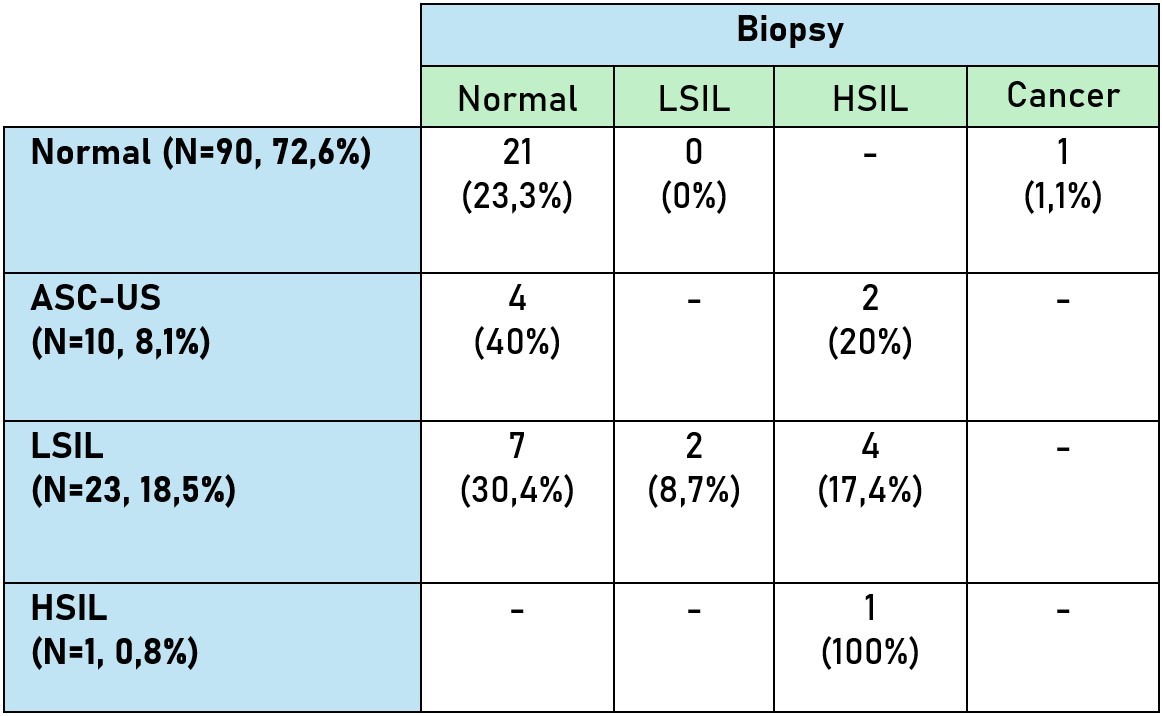
Results: There were 124 patients, 98 (79%) of them were kidney recipients and 26 (21%) were liver recipients. The median age at first screening fo the whole cohort was 37,50 (17,25-67,08) years and median age at first screening for those with atypical cytology was 35,50 years (20,92-56,50). Total detection rate of an atypical cervical cytology was 27,4%. Detection rate of atypical cytology with the conventional smear was 11,1% (n=2) and with liquid based was 30,5% (n=32) [p=0,090]. Number of ASC-US was 10 (29,4%), LSIL was 23 (67,6%) and HSIL was 1 (2,9%). Of 124 patients in the cohort, 42 (33.9%) underwent biopsy. 32 (76,2%) had normal biopsy results, 2 (4,8%) had LSIL, 7 (16,7%) had HSIL and 1 (2,4%) had cancer. 9 (90%) patients with a cervical intraepithelial lesion had a LEEP (Loop Electrosurgical Excision Procedure) and 1 (10%) patient had Hysterectomy. 2 (100%) patients with LSIL had persistence and only 1 (50%) of them had progression to HSIL 46 months after detection of atypia. 5 (71,4%) patients with HSIL had persistence of their lesions and none of them had progression.
Conclusions: Incidence of cervical intraepithelial neoplasms in this patient group is higher compared to the healthy population so we believe the employment of different strategies might be beneficial.