
Prof. Mirza Naqi Zafar, PhD.
Professor of Pathology and Transplant Immunology
Head of Research and Publication. SIUT, Karachi.
I graduated from the University of London in 1975 and completed PhD in 1979. Currently, my research interests are living donor follow-up care where donors have been followed up yearly in a dedicated clinic, and transplant Immunology where the focus has been on HLA matching, Antibody-mediated rejection, HLA-driven immunosuppression, and transplant outcomes. I have authored more than 100 publications and 4 book chapters. I am honored to author a chapter with the late Prof. Paul Terasaki. Currently, I am an Advisor to the Council of The International Society of Organ Donation and Procurement, Secretary General of the Transplantation Society of Pakistan, Secretary of the Nephrology Urology and Transplant Society of SAARC countries, member Ethics Committee, Asian Society of Transplantation, and member of the American Society of Histocompatibility and Immunogenetics. In August 2022, I was invited to give TTS Masterclass on “HLA matching in living-related transplants. Is it justified?” In August 2023, I was featured in the Member Spotlight in the ASHI newsletter.
HLA-driven immunosuppression in living-related kidney transplantation. A protocol for low-income countries
Mirza N Zafar1, Tahir Aziz2, Abdul Rauf3, Adibul Hasan Rizvi4.
1Pathology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 2Transplantation, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 3Transplantation, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 4Urology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan
Introduction: Human Leucocyte Antigen (HLA) matching is considered one of the key determinants of renal graft outcomes in living and deceased donor transplants. The mainstay of maintenance immunosuppression in high-income countries is Tacrolimus (TAC)/Mycophenolate Mofetil (MMF)/Steroids while Cyclosporine (CYA)/Azathioprine (AZA)/Steroid is used in low-income countries. The main reasons for this difference are costs and availability of drugs. This paper presents an immunosuppression protocol based on HLA matching for first living related donor kidney transplants and the graft outcome benefits of this strategy.
Patients and Methods: Between 2007-2020, 4566, first living donor transplants were performed at our center and reported to the Collaborative Transplant Study (CTS) in Heidelberg. HLA matching was performed by molecular methods. Immunosuppression: Group A (0-3 HLA mismatch), CYA (6-8mg/kg) and (8mg/kg in children ≥12), AZA (1.5mg/kg), Steroids (0.5mg/kg) and (1mg/kg in children). Group B (4-6 HLA mismatch), PRA >30% and children <12 years TAC (0.15mg/kg), MMF (10-15mg/kg) and Steroid (0.5mg/kg). Adults were given Antithymocyte globulin (ATG) (3-5mg/kg) for 5 days. Children ≤12 years were given IL-2 Interleukin-2 antagonist 20mg at day 0 and 4. Adults > 50 years irrespective of HLA match were given TAC/MMF/and Steroids. All graft dysfunctions were evaluated by biopsy. The long-term graft survival was compared with outcomes in Europe in the same period 2007-2020 courtesy of CTS. Data was analyzed using SPSS version 22.0.
Results: Of the 4566 transplants, 4044 (88.5%) (Group A) were on CyA/AZA and Steroid, and 522 (11.4%) Group B was on TAC/MMF/Steroid. The mean recipient age in Group A was 28.81±10.52 vs 32.29±9.2 yrs in Group B (p<0.001). The mean donor age in Group A was 34.28±9.6 vs 33.02±8.22 yrs in Group B (p=0.005). The mean HLA mismatch in Group A was 1.83±1.3 vs 4.10±1.4 in Group B (p<0.001). Acute Rejection in Group A (18%) vs (17%) in Group B (p=0.535). Overall One and 5-year graft survival in Group A was 97.75% and 89.9% vs Group B 97.8% and 90.4% respectively (p<0.72). The cost of a 1-year CyA/AZA/Steroid was $650 vs $1,300 for TAC/MMF/Steroid. Graft survival rates were comparable between Europe and our institute vis a vis Induction therapy, Calcineurin inhibitors, and IMPDH inhibitors are given in the Table.
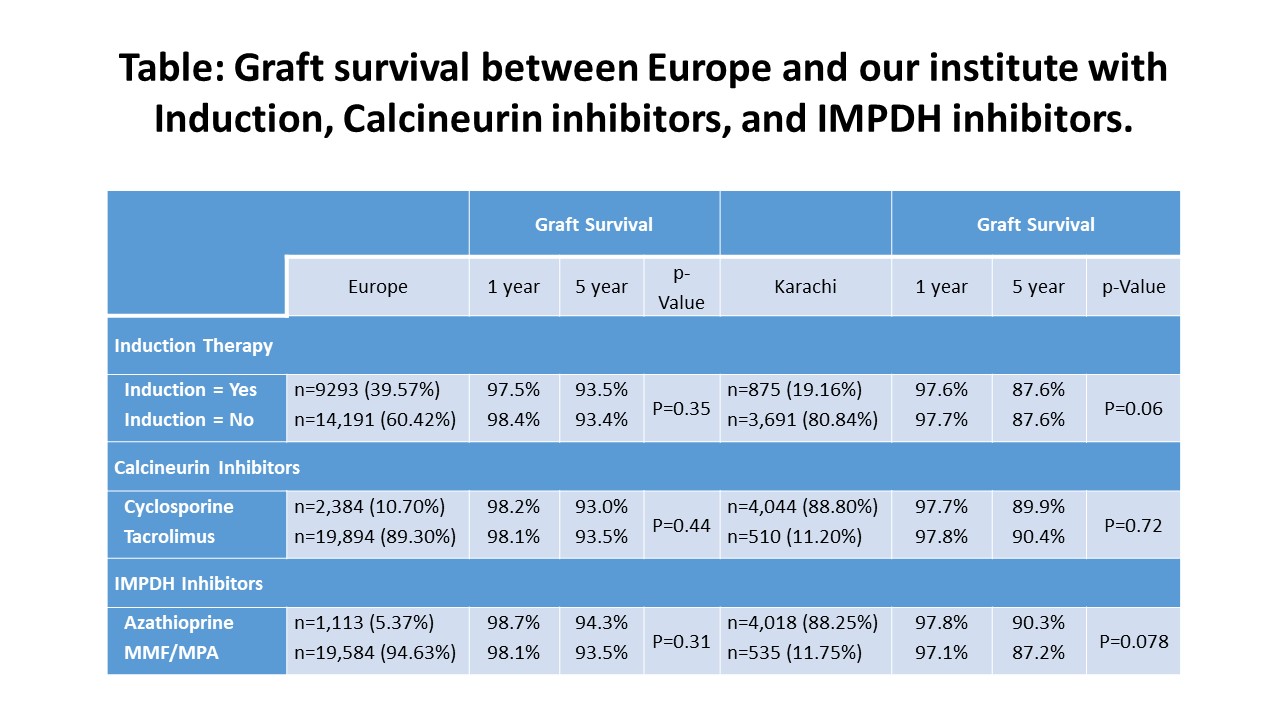
Conclusions: HLA-driven immunosuppression using TAC/MMF/Steroids in poorly matched transplants enabled our center to improve graft survival rates similar to well-matched transplants. The use of more potent immunosuppression only for poorly matched transplants is economical and achieves comparable graft survival rates.
Hein Tran Collaborative Transplant Study (CTS) Heidelberg, Germany, for providing institutes graft survival data for the period 2007 to 2020 and similar data for first living donor transplant in Europe for the period 2007 to 2020.
[1] HLA Match
[2] Immunosuppression
[3] Kidney Transplant
[4] Graft Survival
