Timing is (Almost) everything: The relationship between deceased donor PaO2/FiO2 ratio and lung graft survival
Darren Stewart1, Jessica M Ruck2, Phil Sommer4, Allan B Massie1,3, Dorry L Segev1,3, Luis Angel4.
1Surgery, NYU Langone Health, New York, NY, United States; 2Surgery, Johns Hopkins University, Baltimore, NY, United States; 3Population Health, NYU Langone Health, New York, NY, United States; 4Transplant Institute, NYU Langone Health, New York, NY, United States
Purpose: The donor PaO2/FiO2 ratio (PFR) is highly associated with lung utilization yet often fails to manifest as a significant risk factor of lung graft failure in published studies. Though selection bias may play a role, this apparent lack of association may also stem from the most commonly studied PFR value (from the Deceased Donor Registration (DDR) form) not necessarily being obtained with conventional ventilator settings nor subsequent to donor management practices that can improve lung physiology.
Methods: Using U.S. Organ Procurement & Transplantation Network (OPTN) registry data, we studied 26,361 age ≥12 lung-alone recipients transplanted 1/2010-6/2022. In addition to the DDR PFR, we used serial arterial blood gas (ABG) data from DonorNet to identify PFRs with a positive end-expiratory pressure (PEEP) of 5 measured closest to Admission, Authorization, Allocation Start, Last Serial, and Last Serial @100% FiO2. We used propensity-weighted Kaplan-Meier and Cox regression to evaluate the relationship between PFR and long-term graft survival, adjusting for 10 covariates associated with graft outcomes and PFR. PFR was parameterized dichotomously (<300, 300+) in the primary analysis, and in 4 levels and continuously in secondary analyses.
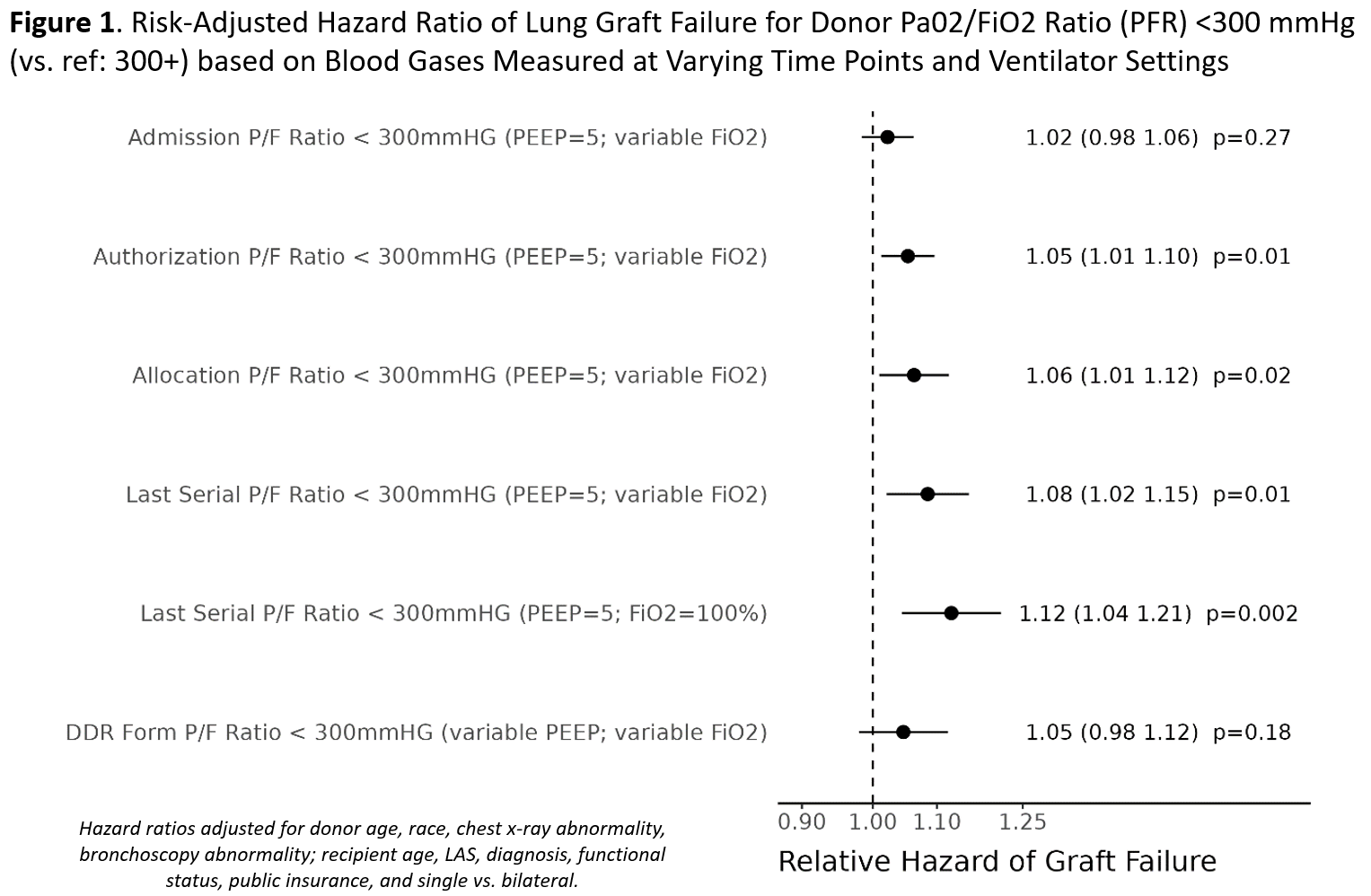
Results: Of transplanted lungs, PFR was <300mmHg for 33.3% at Admission; 6.3% at Last Serial @100% FiO2; and 7.7% on the DDR. Neither Admission (aHR=1.02, p=0.27) nor DDR (aHR=1.05, p=0.18) PFR was associated with graft survival. However, a last PFR @100% FiO2<300 was associated with a 12% higher graft failure risk (p=0.002; Fig 1) and a median graft half-life (5.4 yrs; 95% CI: 5.0, 5.9) nearly 1 year shorter than with PFR 400-500 (6.3; 6.1, 6.5).
Graft survival was similar at PFR of 400 (aHR=1.02; 0.95, 1.09) vs. 600, suggesting diminishing returns with further PFR increases (Fig 2A).
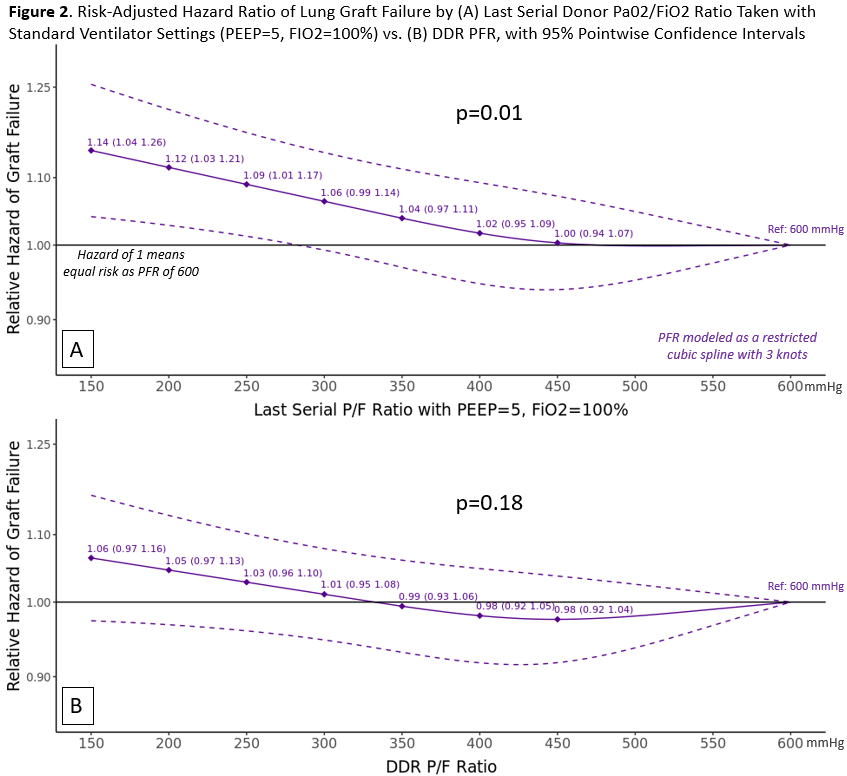
Conclusions: Studies suggesting PFR has no implications for lung graft survival may be misleading. Though U.S. OPOs are required to report ABGs with PEEP=5 within 2 hours of lung offers to support transplant center decision-making, PFRs measured later during donor management are more highly associated with graft survival and thus may better reflect underlying organ quality and graft prognosis. PFR increases above 400 may provide minimal, if any, incremental survival advantage.
[1] lung
[2] P/F ratio
[3] donor management
[4] donor evaluation
[5] donor quality
[6] graft survival
