Exploring acceptability of lung uDCD among clinical and community stakeholders in New York City
Jingzhi Xu1, Carolyn Sidoti1, Mariam Girgis1, Luis Angel1, Stephanie Chang1, Justin Chan1, Brendan Parent1, Macey Levan1, Robert Montgomery1, Stephen Wall1.
1Surgery, New York University School of Medicine, New York City, NY, United States
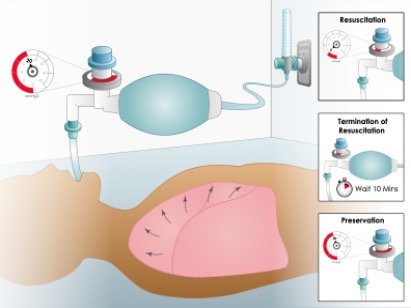
Introduction: The Toronto lung uncontrolled donation after circulatory death (uDCD) protocol used partial inflation with 20 cm H20 positive end-expiratory pressure and oxygen to preserve lungs noninvasively for up to 3 hours with 36% transplant yield after ex-vivo lung perfusion. The protocol required obtaining authorization for organ donation before lung preservation causing median 166 min delays in initiation. Transplant yield could markedly improve if authorized decision-makers within opt-in donation systems accept initiating noninvasive lung preservation without requiring prior permission. The study purpose was to vet this approach with clinical & community stakeholders in New York City (NYC).
Methods: This qualitative focus group study occurred from July 2022 to March 2024 with community health workers and religious leaders served by and clinician working in emergency departments and ICUs of NYU Langone Brooklyn and Manhattan Hospitals. Participants were purposefully recruited to balance race/ethnicity, religious, and stakeholder groups. Moderators explained noninvasive lung preservation would begin without requiring prior permission regardless of organ donor registration status. For those without first person authorization, decision-makers could cease preservation or contemplate donor authorization. Participants discussed ethical permissibility of clinical procedures and authorization processes pertinent to stakeholders. Afterwards, participants completed demographic surveys with a 5-pt Likert question about support for the program. Digital audio recordings were transcribed verbatim and coded with NVivo (1.7.1). Iterative coding discerned themes, theoretical constructs, and summary narratives. Recruitment occurred until achieving thematic saturation.
Results: We held 17 focus groups with 85 participants (3 to 8 per group). Of these, 84 (98.8%) supported the program. Among participants, 60% were female with nearly equal representation by race/ethnicity, religious, and stakeholder groups. Themes emerged representing clinical, ethical, legal, logistical, and public concerns. Clinical stakeholders voiced support for the program, but maintaining separation of clinical and preservation teams required personnel from other locations to initiate organ preservation expeditiously and have conversations with families. Clinical and community stakeholders mostly supported initiating preservation without prior permission, stating they “… will not be offended because it is saving somebody’s life.” Those initially voicing opposition supported the program after discussion. Most persons of faith were supportive even among those whose religions oppose brain death diagnosis. Participants voicing mistrust with organ donation believed the lung uDCD program was not offensive.
Conclusions: Community and clinical stakeholders in NYC mostly voiced support for lung uDCD and initiating noninvasive lung preservation without requiring prior permission.
National Institute of Health R61/R33 HL156890 .
[1] Uncontrolled donation after circulatory death
[2] uncontrolled donation after cardiac death
[3] qualitative research
[4] deceased organ donation
[5] lung preservation
