Pediatric lung transplantation in China, 2019-2023
Xiaoshan Li1, Jingyu Chen1.
1Lung Transplantation Center, the Affiliated Wuxi People's Hospital of Nanjing Medical University, Wuxi, Jiangsu, People's Republic of China
Lung Transplantation Center of Wuxi City in China.
Background: Pediatric lung transplantation (pLTX) is a relatively rare operation and its epidemiology and impact on survival are still understudied in China. This study was aimed to describe the characteristics and survival outcomes of pLTX in China.
Methods: This retrospective study analyzed data of pLTX recipients aged £17 years between January 2019 and December 2023 from the China Lung Transplantation Registry (CLuTR). Pre-operative, intra-operative, post-operative complications and survival rates were described.
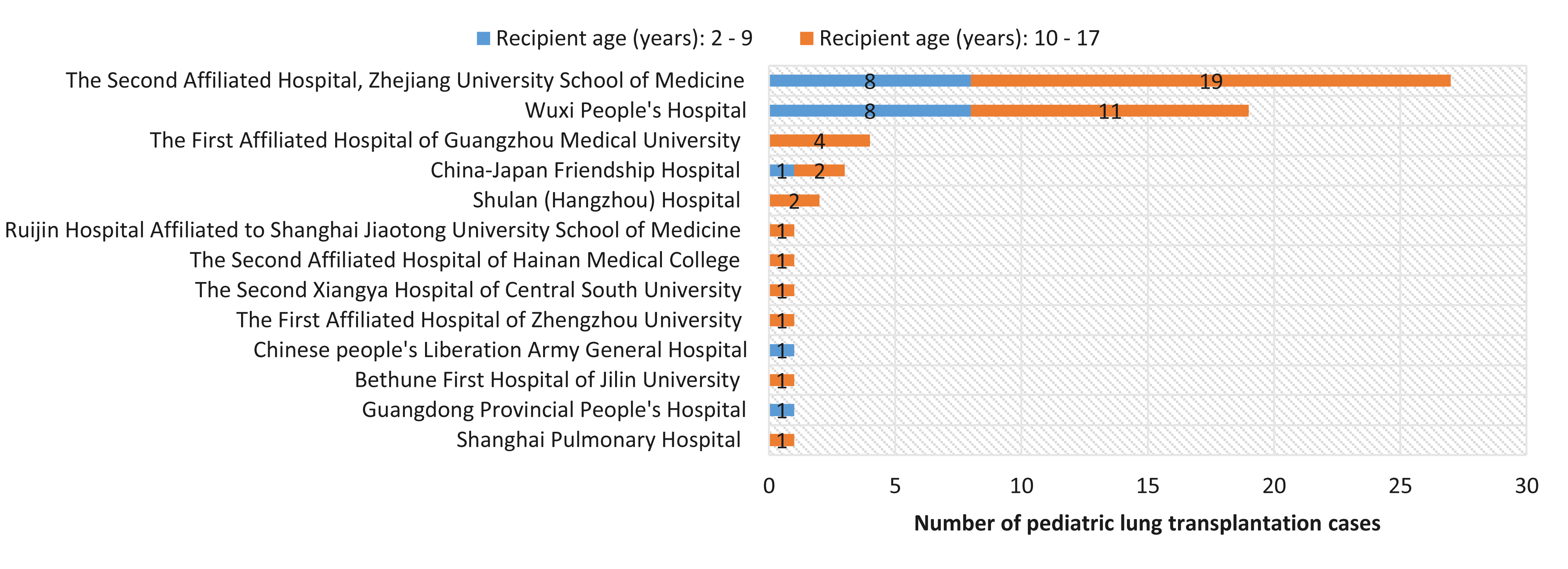
Results: A total of 63 transplants were performed in 62 pediatric patients in 13 hospitals during the study period. The annual number of pLTX increased from 9 in 2019 to 22 in 2023 in China. The 73.0% transplants were performed in the Second Affiliated Hospital, Zhejiang University School of Medicine (n=27) and Wuxi People's Hospital (n=19).
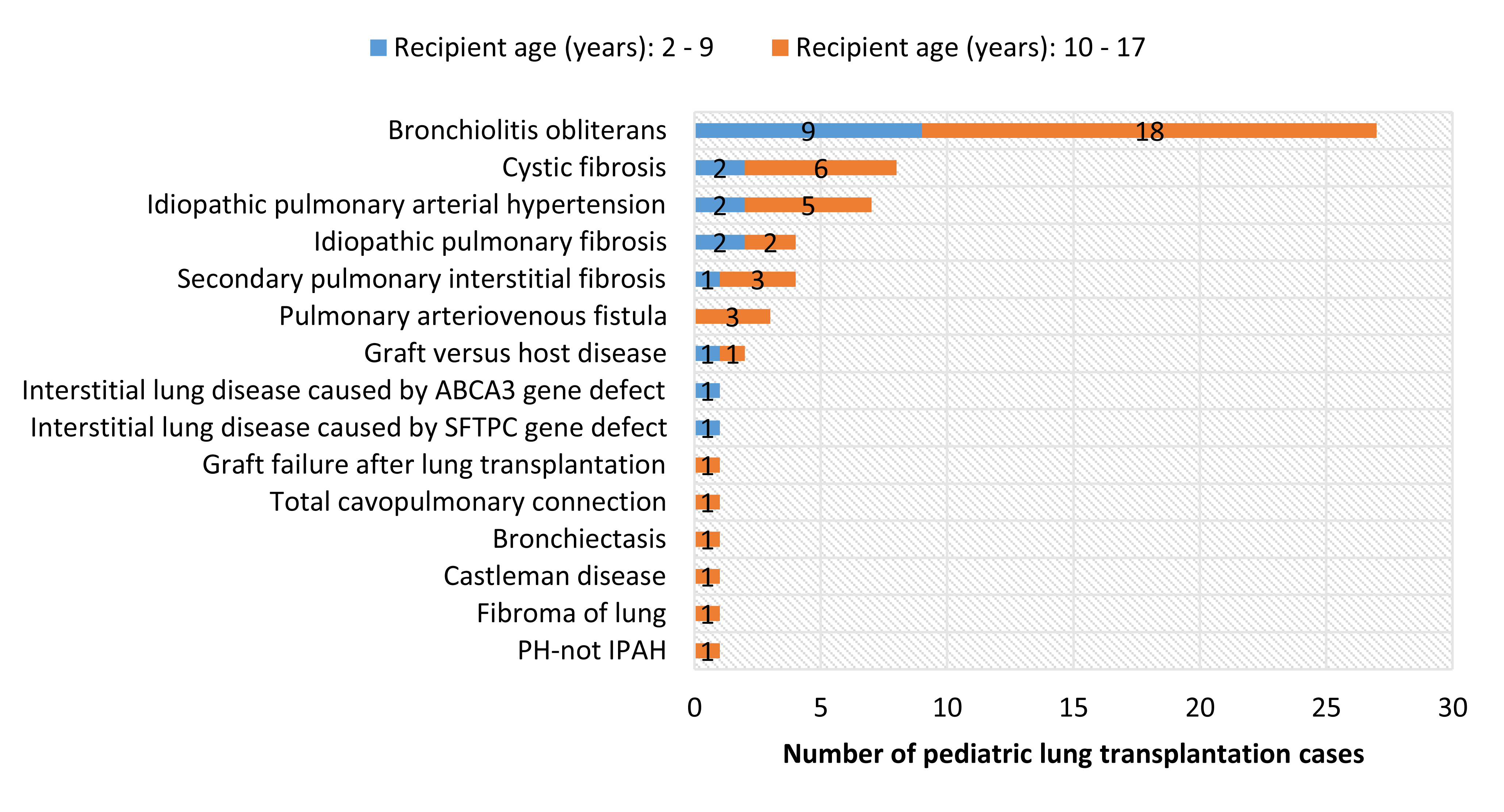
The 48.4% were males and aged 2-9 years accounted for 30.6%. The primary indications were bronchiolitis obliterative (42.9%), followed by cystic fibrosis (12.7%), idiopathic pulmonary arterial hypertension (11.1%), idiopathic pulmonary fibrosis (6.3%), and secondary pulmonary interstitial fibrosis (6.3%).
Almost all (96.8%) pLTX were bilateral transplant, and 69.4% used extracorporeal membrane oxygenation (ECMO).
Infection was the most common complication after pLTX (63.8%), followed by acute kidney injury (18.6%), primary graft failure (13.6%), arrhythmia (10.3%), heart failure (10.2%), and acute liver injury (10.2%). The incidence of tracheal anastomotic stenosis was higher among recipients aged 2-9 years than that in recipients aged 10-17 years (21.1% vs 2.5%, P=0.033). Among 62 recipients, the survival rate at hospital discharge was 83.3%. The median (interquartile range) length of hospital stay and intensive care unit stay among 50 survivors was 33.5 (21.0~54.0) days and 6.0 (3.7~13.6) days, respectively. ECMO was used among 28 recipients after surgery, and the use of ECMO was more common among recipients aged 10-17 years compared to those aged 2-9 years (60.0% v.s. 21.1%, P=0.005). The median follow-up time of 63 pediatric recipients was 324.5 (IQR: 97.5-983.3, range: 4-1756 days. The 30-day, 90-day, 180-day, and one-year survival rates and 95% confidence intervals after surgery was 93.5% (87.6-99.9), 83.8% (75.1-93.5), 80.1% (70.6-90.9) and 80.1% (70.5-90.9), respectively.
Conclusion: Our findings contribute to the understanding of the trends, indications, donor and recipient characteristics, and complications of pLTX in China. Despite its small size, pLTX is growing gradually with favorable outcomes. Future research on the long-term follow-up of pLTX recipients is needed to examine factors associated with prognosis of pLTX.
We are grateful to all lung transplant hospitals for providing data to the CLuTR, which enabled this study to proceed smoothly. Thanks to the Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (BJ2023016) for the financial support of this research.
[1] Lung transplantation
[2] Pediatric lung transplantation
