Fluid management during pediatric lung transplantation: Single-center experience
Ge Luo1, Min Yan1, Lifang Zhang1, Yuanyuan Yao1, Man Huang2, Jingyu Chen3.
1Anesthesiology, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, People's Republic of China; 2Intensive Care Unit, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, People's Republic of China; 3Lung Transplantation, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, People's Republic of China
Background: The impact of intraoperative fluid balance on postoperative outcomes in pediatric lung transplantation (LTx) has not been proven yet. This study aimed to preliminarily investigate the impact of fluid balance on postoperative outcomes in pediatric LTx and to share experiences in fluid management.
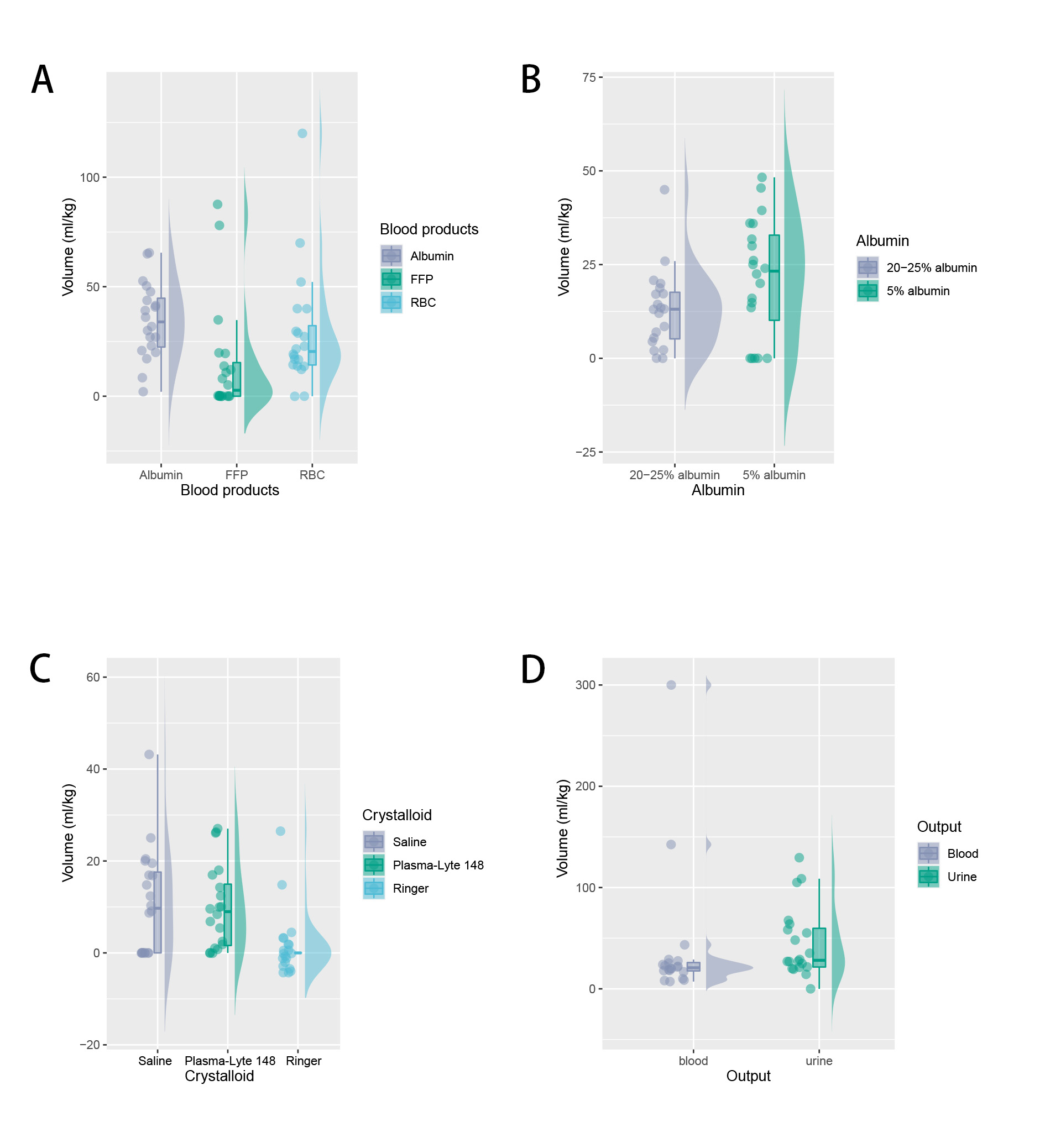
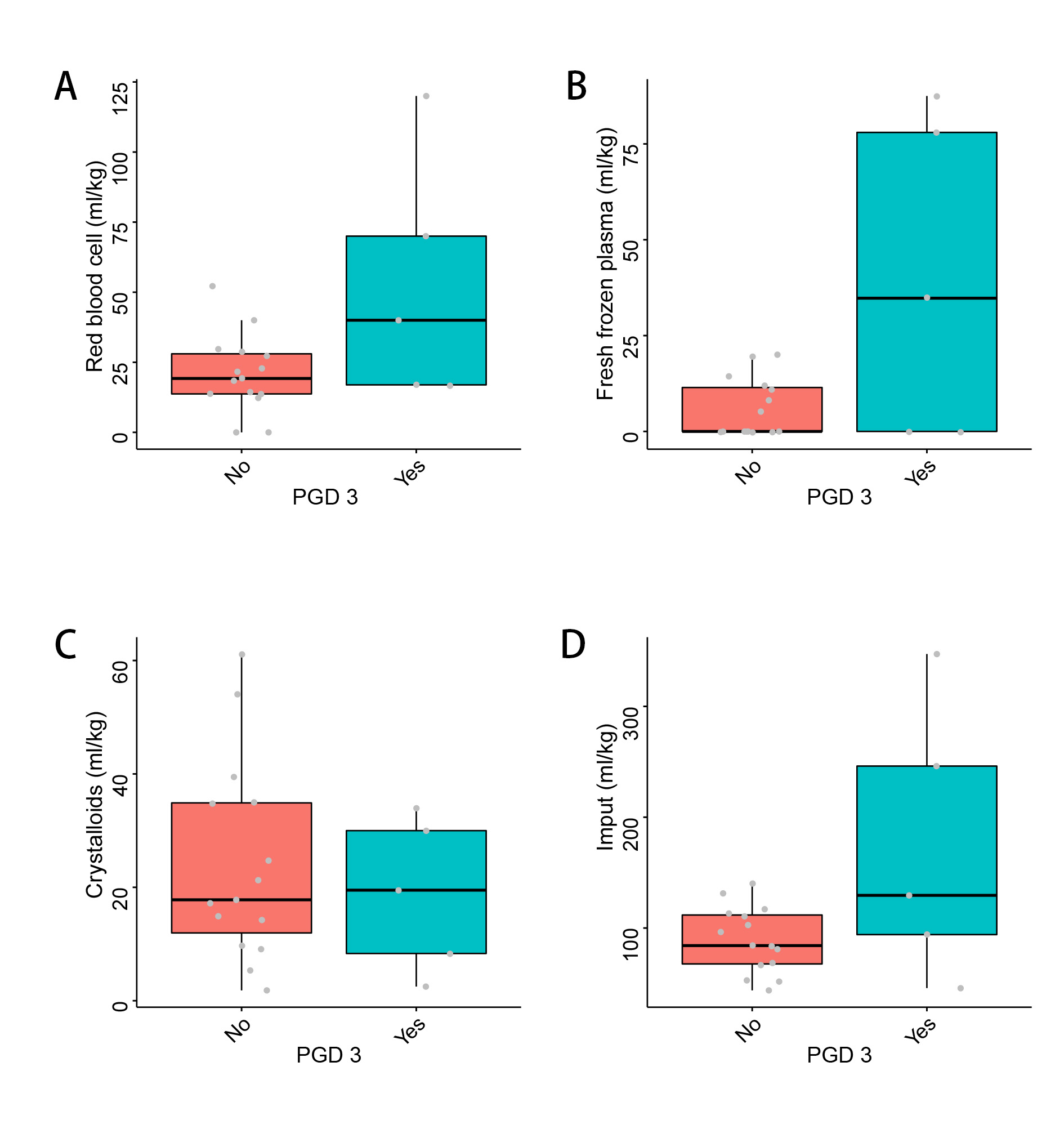
Methods: We analyzed the reports of children who underwent LTx from July 2019 to August 2023. Fluid overload (FO) was defined as an intraoperative fluid balance greater than or equal to 10%. Twenty children were classified into the FO (n=12) and non-FO (n=8) groups, and differences in postoperative graft dysfunction (PGD) and other outcomes were compared between the two groups.
Results: The results showed no significant difference in the incidence of postoperative adverse outcomes between the two groups (P>0.05). The results remained consistent even when the threshold was raised to 20%. Although blood product transfusions and fluid intake were higher in children from the PGD group than in the non-PGD group, the differences were not statistically significant (P>0.05).
Conclusions: The available evidence is not sufficient to suggest that the non-FO approach in the restrictive fluid strategy can reduce the risk of adverse outcomes after lung transplantation in children, but it did not mean that FO strategy should be encouraged. Further high-quality clinical studies must be conducted to support these findings.
[1] Pediatric
[2] lung transplantation
[3] fluid management
