Pediatric kidney transplantation in infants and low-weight children: What have we learned so far?
Basak Akyollu1, Cemile Pehlivanoglu2, Ozlem Unlugedik2, Cihan Karatas1, Emre Arpali3, Ilmay Bilge2, Burak Kocak1.
1Organ Transplantation, Koc University Hospital, Istanbul, Turkey; 2Pediatric Nephrology, Koc University Hospital, Istanbul, Turkey; 3Organ Transplantation, Medical College of Wisconsin, Milwaukee, WI, United States
Introduction: Kidney transplantation (KTx) in low-weight children and infants using larger living donor adult kidneys is a challenging surgery with special characteristics.
Method: This is a single center retrospective study reviewing pediatric KTxs in terms of indications, concomitant surgery, techniques and postoperative complications. Patient and graft survivals were calculated with Kaplan-Meier survival analysis.
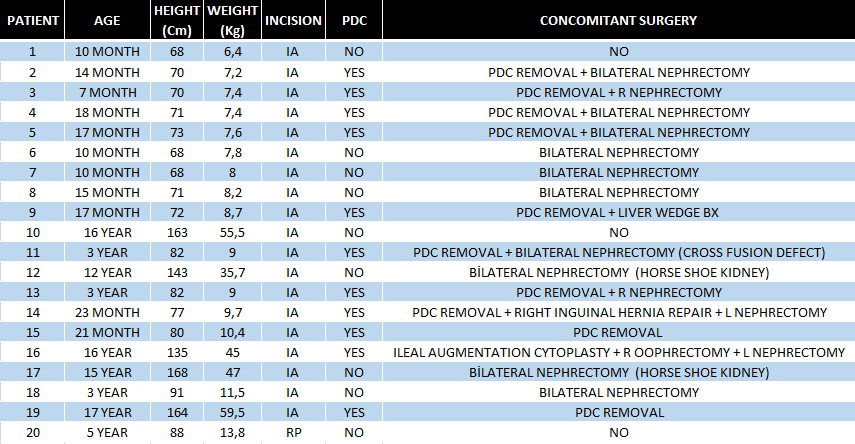
Results: Between July 2008 and December 2023, 112 children underwent living-related KTx. Median recipient age was 8,5 (range 0,6-17,4)years with median body weight of 21,6 (range 5,9-93)kg. Body weight was <15 (range 0,9-14,6)kg in 37 of the 112 patients (33,3%). Standard retroperitoneal approach (RP) was utilized in 75 (67%) of the patients. 22 (29,3%) of these incisions were done by extended hockey stick incision whereas the rest 53 (70,6%) were done with standard hockey stick incision. Intraabdominal approach (IA) was utilized in 37 (33%) of the cases. Bilateral or unilateral native nephrectomy (NNx), augmentation ureterocystoplasty or enterocystoplasty, peritoneal dialysis catheter (PDC) removal were done concomitantly in 56 (50%) of the cases. Depending on the recipient’s diameter of vessels and vascular size match with the donor kidney’s vasculature, selected anastomosis sites were reported in Table1.
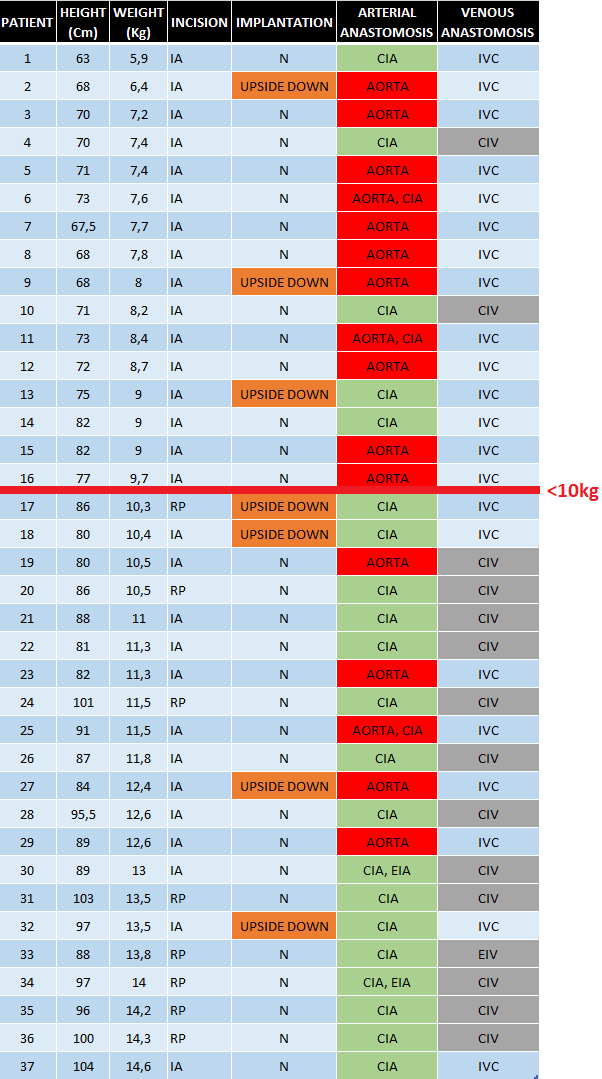
To achieve the best anatomical placement to secure a safe vascular anastomosis, upside down implantation technique was used in 10 of the patients (9%). No arterial/venous thrombosis was seen. IA was the choice in 7 of these 10 recipients. We used partial right liver mobilization to place the allograft in the retro-hepatic area when there was size mismatch between the donor kidney and recipient in low-weight children. We put a drain especially in small kids (IA) with PDC in order to avoid compartment syndrome (Table2).
Overall patient and graft survivals are 98,2% and 97,3%, respectively at 20,6 (range 0,4-66,5) months.
The most frequent post-operative surgical complications seen in our series was intestinal obstruction (n=3). 2 of them had a concomitant NNx and one of these 2 patients had also developed urine leak (n=1) which required laparotomy during the follow up and the other one had a history of a previous intraabdominal surgery naming left surrenalectomy for a neuroblastoma 3 years before the KTx. The third case who had a history of bilateral NNx in an outer center 2 years before KTx due to Wilms tumor, whose KTx was performed by RP, developed ileus at post-operative day 5 which also required laparotomy. The other complications were evisceration (n=1) and surgical site hemorrhage (n=1) which received red blood cell transfusion as the sole management for the bleeding.
Conclusion: Pediatric KTx is a challenging procedure especially in low-weight children and infants but can be carried out safely with manageable morbidities with specific surgical modifications.
[1] Kidney Transplantation
[2] Pediatric
[3] Infants
[4] Low-weight children
