Infection transmission risk from kidney donors with active Hepatitis B: A systematic review and meta-analysis of observational data
Karen Waller1,2,3, Rachel Davies1, Emma Garrett1,4, James Hedley1, Kate Wyburn1,5, Angela Webster1,3,6.
1Collaborative Centre for Organ Donation Evidence, Sydney School of Public Health, University of Sydney, Camperdown, Australia; 2Department of Gastroenterology and Hepatology, Concord Repatriation General Hospital, Concord, Australia; 3NHMRC Clinical Trials Centre, Faculty of Medicine and Health, University of Sydney, Camperdown, Australia; 4School of Medical Sciences, Faculty of Medicine and Health, University of Sydney, Camperdown, Australia; 5Department of Renal Medicine, Royal Prince Alfred Hospital, Camperdown, Australia; 6Department of Renal Medicine, Westmead Hospital, Westmead, Australia
Aims: Potential kidney donors with active hepatitis B (HBV), defined as positive surface antigen (HBsAg) and/or nucleic acid test (NAT), are usually declined for HBsAg-negative recipients. With vaccination and antivirals, transplantation could be safe. We aimed to quantify the transmission risk.
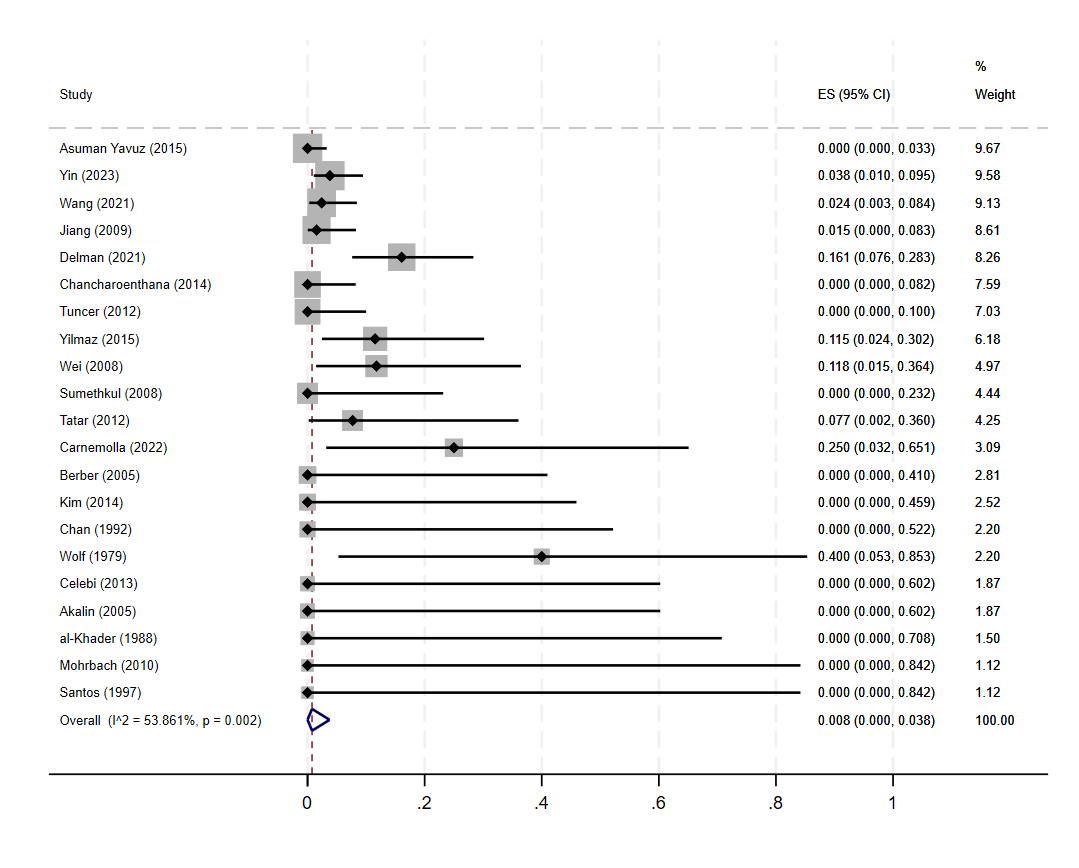
Methods: Systematic review and meta-analysis, searching MEDLINE for “hepatitis B” and “kidney transplantation”. We included cohorts of kidney transplantation from donors with active HBV to HBsAg-negative recipients. Transmission was defined as HBsAg or HBV NAT positivity post-transplant. Transmission proportions were pooled using meta-analysis with random effects, employing Freeman-Turkey double arcsine transformation and exact 95% confidence intervals.
Results: After screening 3,143 records, 21 cohorts were included. Among 606 donors, most were living (57%); all had positive HBsAg but most had negative NAT (55%). Among 614 recipients, most had protective surface antibody (HbsAb, 86%) titres, and many were core antibody positive (48%). Prophylaxis varied in strategy (8 cohorts universal, 6 none), type (hepatitis B immunoglobulin 37% recipients, antivirals 44%) and duration. There were 26/614 HBV transmissions (4.2%), less common where all recipients had protective HBsAb (1.3%) or all donors had negative NAT (0.6%). There were 3 deaths due to HBV (0.5%): all occurred off prophylaxis (one never given, one post short course, and one non-compliant). The pooled transmission rate was 0.8% (95%CI: 0.00-3.8%, Figure 1) although there was substantial heterogeneity between studies (I2=53.9%). This may be explained by differences in case ascertainment, prophylaxis strategies or donor/recipient factors.
Conclusion: Given low transmission rates, donation could be considered from kidney donors with active hepatitis B in controlled circumstances.
[1] hepatitis B
[2] meta-analysis
[3] organ donors
