Hypothermic oxygenated machine perfusion is not associated with an increased risk of infection in the recipient: A retrospective single-centre cohort study
Silvia Corcione1,2,4, Nour Shbaklo1, Maria Roberta Fortunato3, Danilo Vinci3, Renato Romagnoli2,3, Francesco Giuseppe De Rosa1,2, Damiano Patrono3.
1Infectious Diseases, Department of Medical Sciences, AOU Città della Salute e della Scienza di Torino, Turin, Italy; 2School of Medicine, University of Turin, Turin, Italy; 3General Surgery 2U - Liver Transplant Unit. Department of Surgical Sciences, AOU Città della Salute e della Scienza di Torino, Turin, Italy; 4Tufts University School of Medicine, Tufts University, Boston, MA, United States
Background: Use of machine perfusion (MP) in liver transplantation (LT) is gaining widespread acceptance. One potential drawback of MP is the risk of graft contamination due to the increased manipulation and exposure, determining infection in the recipient. Bacterial overgrowth resulting in severe recipient sepsis has been well documented during normothermic machine perfusion, but data on hypothermic oxygenated machine perfusion (HOPE) are scarce. Aim of this retrospective study was evaluating the risk of blood stream infection in recipient following HOPE versus static cold storage (SCS).
Methods: Adult (≥ 18-year-old) LT recipients transplanted in the period March 2016 - June 2023 were included. Exclusion criteria were redo-LTs, combined transplant, urgent LT, hospital admission at LT, treatment by temporary packing and delayed abdominal wall closure, use of normothermic MP or normothermic regional perfusion. 1:1 propensity score (PS) matching was used to overcome selection bias. PS were calculated based on MELD-Na, ascites, donor age, LT operation time, and number of packed red blood cells (PRBC) transfused during LT. Cultures of preservation fluid samples obtained during backtable preparation were available for all patients. Data on microbiological isolates and infection episodes in LT recipients were recorded from electronic clinical charts. Antibiotic prophylaxis with piperacillin/tazobactam was administered regardless of HOPE use for 72 hours unless otherwise indicated based on donor or recipient cultures. Antifungal prophylaxis with amphotericin B was selectively administered according to our institution protocol.
Results: 709 (SCS, n=523; HOPE, n=186) out of 1062 patients were selected from the original cohort after exclusion. By PS matching, two groups of 185 patients were selected. Groups had comparable MELD-Na (12 vs 12;SMD=0.03), ascites (33.5 vs 31.9%;SMD=0.03), operation time (352 vs 357 min;SMD=0.02) and transfusion requirement (2 vs 2 PRBC units;SMD=0.09). Due to selection bias, patients in HOPE group received grafts from older donors (76.3 vs 74.3 years;p=0.03;SMD 0.10), with higher BMI (26.9 vs 24.9;p<0.01;SMD=0.39) and macrosteatosis (2 vs 1%;p=0.02;SMD=0.28). Overall, 82% of patients had a positive preservation fluid culture, with no significant differences between groups. Isolates were mostly coagulase negative staphylococci.
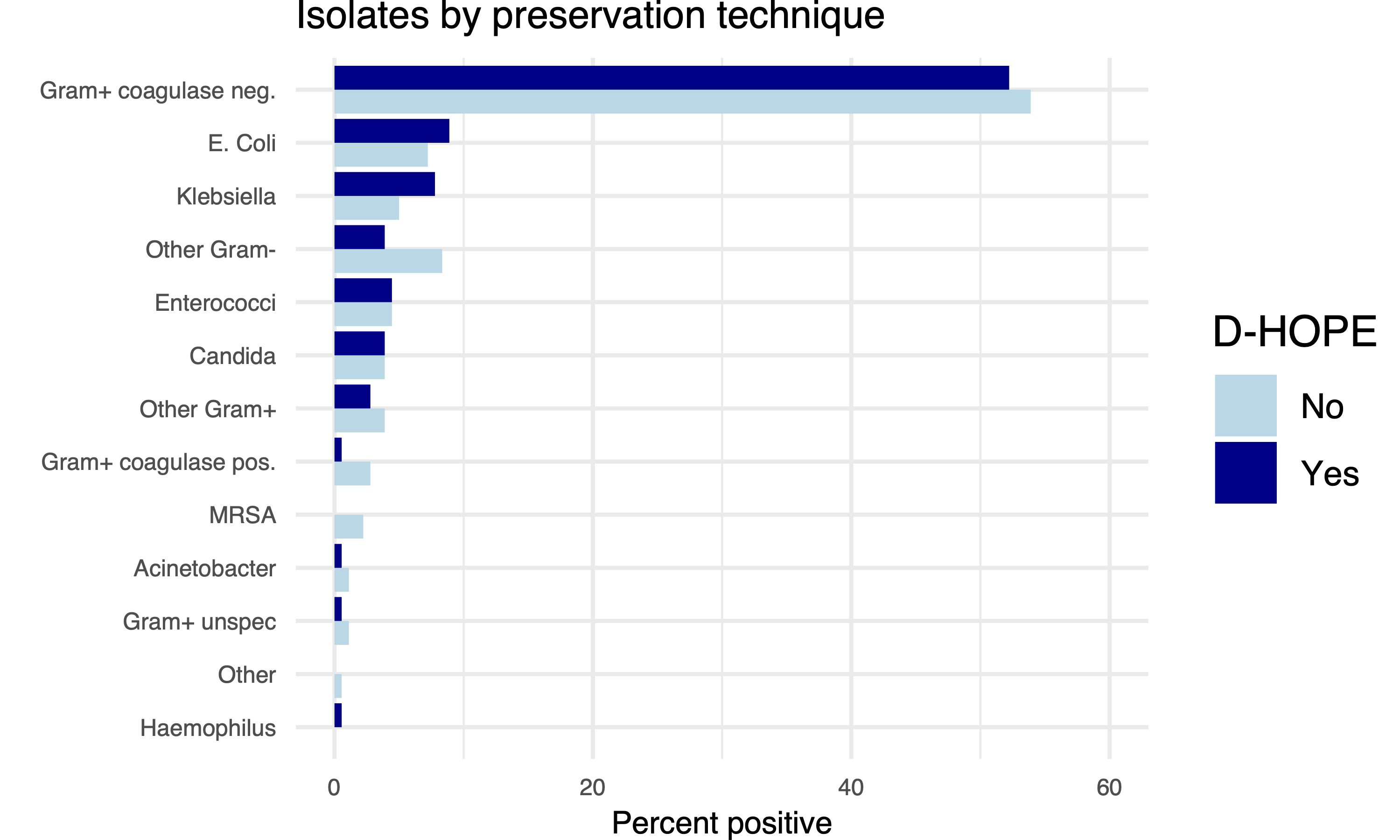
The rate of bloodstream infection after LT were comparable between study groups. Of note, patients in HOPE group presented more positive microbiological samples, mostly from bile or tracheal aspirates, not associated with clinical symptoms.
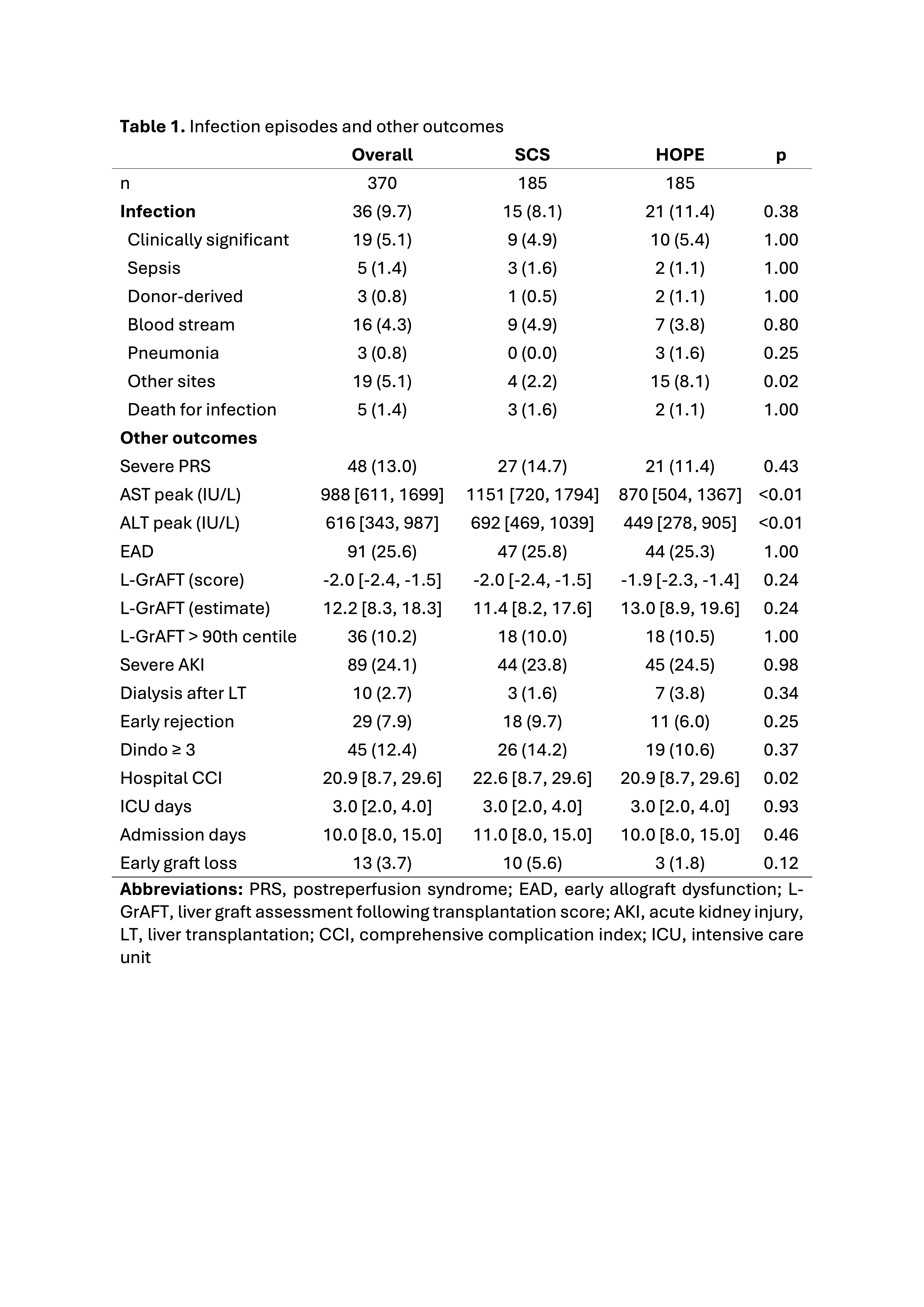
Donor-recipient transmission was anecdotal, with only two cases of recipient bloodstream infection due to donor-recipient transmission of carbapenemase-producing Klebsiella Pneumoniae (HOPE) and Acinetobacter Baumanii (SCS).
Conclusion: HOPE use is not associated with an increased risk of infection and do not require adaptation of antimicrobial prophylaxis after LT.
[1] Machine perfusion
[2] Hypothermic oxygenated machine perfusion
[3] Liver transplantation
[4] Transplant infectious diseases
