Effect of recurrent CMV viremia on graft and patient survival in renal transplantation
Sabina Dobrer1, Karen R Sherwood2, Kimberly Davis3, James Lan1,2, John Gill1, Anat Fisher1, Paul A Keown1,2.
1Department of Medicine, University of British Columbia (UCB), Vancouver, BC, Canada; 2Department of Pathology and Laboratory Medicine, University of British Columbia (UCB), Vancouver, BC, Canada; 3Global Evidence and Outcomes, Takeda Development Center Americas, Inc., Lexington, MA, United States
Background: The Genome Canada Precision Medicine Program has shown that cytomegalovirus (CMV) viral load kinetics determine the risk of failure in a large renal transplant cohort with uniform clinical management followed for up to 13 yrs. Here we show that recurrence of CMV viremia, related to CMV risk status, treatment and other factors, has a further profound effect on graft and patient survival.
Methods: 2,507 sequential patients who received a renal transplant at UBC from 01/01/08-31/12/08 were followed until 31/12/19 (>6 million patient days of follow-up). 1,441 (57%) received a deceased donor (DD) and 1066 (42%) a live donor (LD) transplant, 2321 (93%) received 1 graft and 186 (7%) >1 graft. All were managed using uniform provincial guidelines for immune suppression and anti-viral therapy. Patients were stratified by donor source, graft number, donor/recipient (D/R) CMV status and CMV viral episode for analysis of graft and patient outcomes.
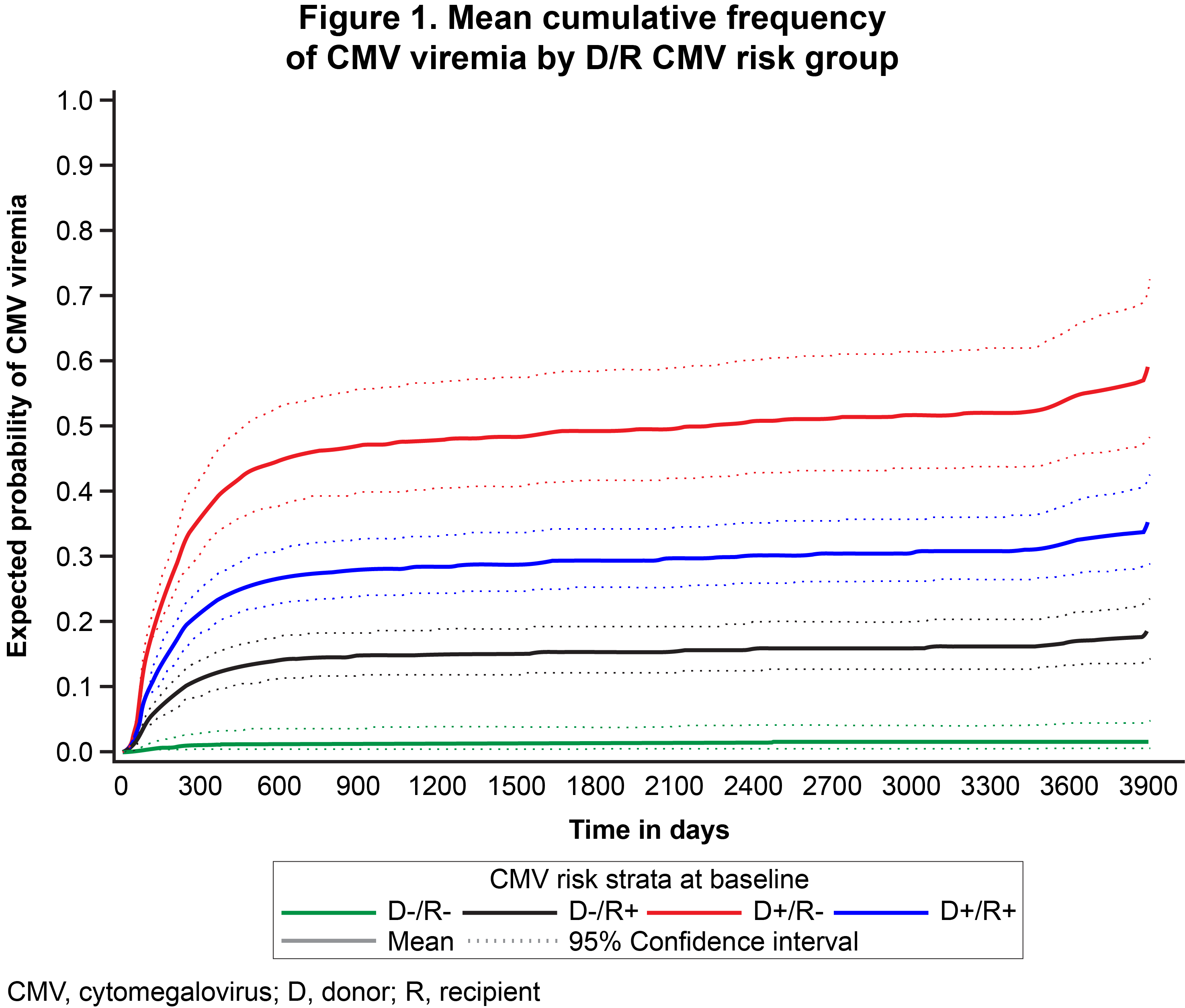
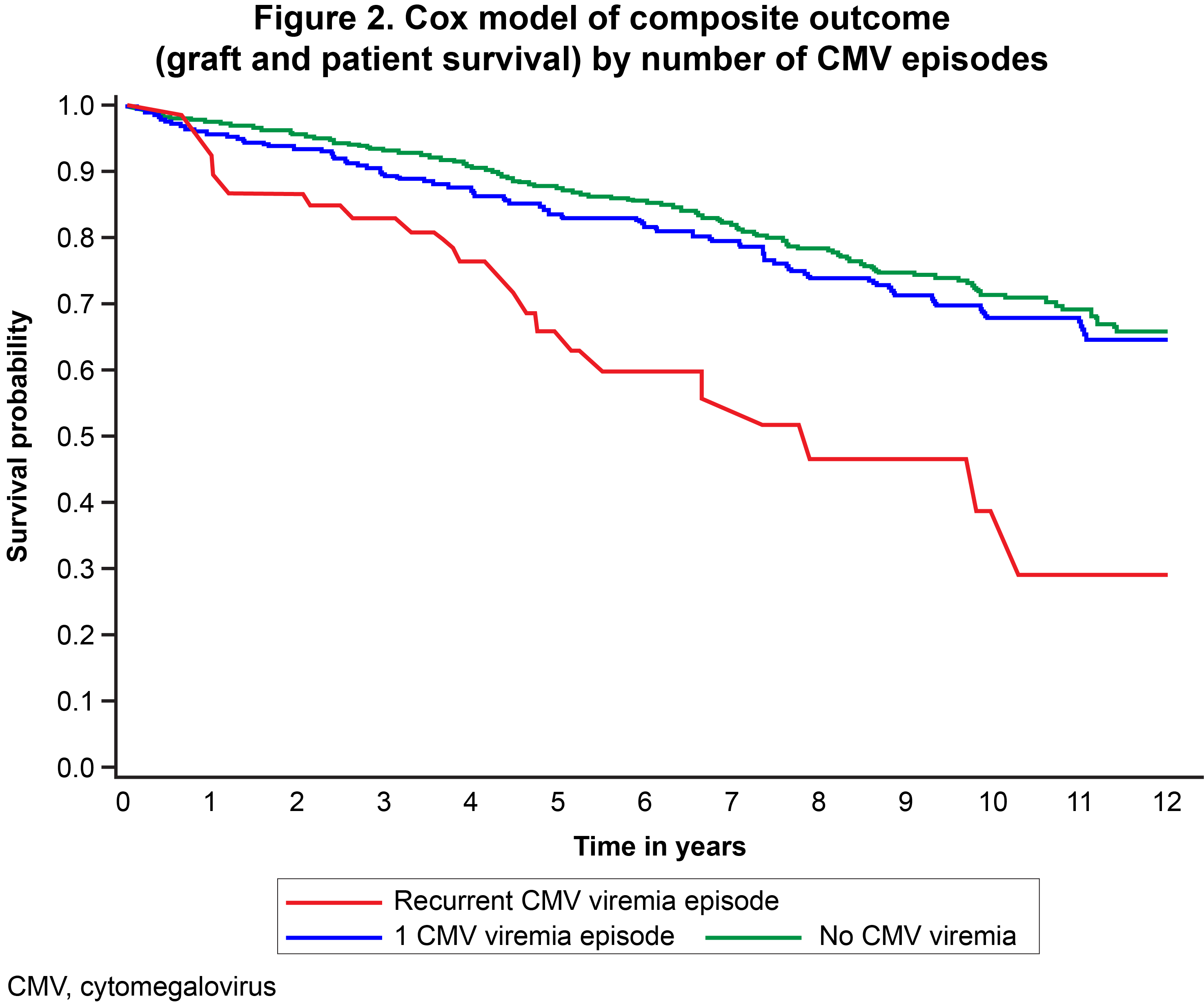
Results: 2,464 patients (98%) had complete data for analysis; 59% were Caucasian, 62% were male, the mean age was 52 ± 15 yrs and CMV strata were D+/R+ (883, 35%), D+/R- (454, 18%), D-/R+ (685, 27%) and D-/R- (442, 18%). Overall, 434 patients developed primary CMV viremia (viral titre: ≥830 IU/ml; range: 1-7 log 10 IU/ml) of whom 67 had recurrent viremia. Recurrent viremia was more common vs no viremia in non-Caucasian (51% vs 39%, p=0.0014), older (mean: 58 vs 51 yr. p<0.0001), D+/R- (45% vs 15%, p<0.0001), and DD graft (78% vs 55%, p<0.0001) recipients, and those receiving antiviral prophylaxis (72% vs 41%, p<0.0001). Multinomial adjusted regression confirmed that increased age, non-Caucasian race, diabetes, D+/R-status and delayed graft function (DGF) were significant predictors of recurrent CMV viremia (p<0.005). Mean peak time from transplant to recurrent CMV infection was 250 days, being shortest in D+/R+ and longest in D-/R- recipients (Figure 1). Mean cumulative event frequency (total viremic episodes by time) reached an asymptote of 21% at 500 days, with rates of 43% in D+/R-, 26% in D+/R+, 14% in D-/R+, and 1% in D-/R- risk groups. Kaplan–Meier analysis found that the probability of the composite endpoint of patient survival with a functioning graft was significantly reduced in patients with recurrent CMV viremia (no CMV viremia 85%, primary CMV viremia 83%, recurrent CMV viremia 63%, p<0.0001; Figure 2).
Conclusion: This study confirms that patients with a recurrence of CMV viremia post-transplant are at exceptionally high risk of transplant failure as measured by graft loss or death. The risk of recurrent CMV is related to race, age, donor source and D/R CMV status. Conventional prophylaxis appears to be inadequate to protect these patients from recurrent infection and its serious consequences, indicating that alternative treatment strategies, with continuous long-term monitoring and rapid, effective therapy are of vital importance in these susceptible patients to maximize transplant success.
Funding provided by Takeda Development Center Americas, Inc., Genome BC (Genome Canada 273AMR) and the Canadian Institutes of Health Research (CIHR GP1-155871) .
[1] Renal transplant
[2] Mortality
[3] Cytomegalovirus
[4] Graft loss
[5] Recurrence
