Nocardiosis in living related donor kidney transplant recipients: A study from a low income country
Sana Jamil1, Salma Batool2, Shazia Rao1, Mirza Naqi Zafar3, Adib Rizvi4.
1Microbiology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 2Molecular Biology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 3Pathology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan; 4Urology and Transplantation, Sindh Institute of Urology and Transplantation, Karachi, Pakistan
Introduction: Nocardiosis represents a unique challenge in the field of infectious diseases especially in immunocompromised individuals. Cotrimoxazole is the first-line therapy for all forms of Nocardiosis, with Imipenem and Minocycline being alternative. However, with increasing sulfonamide resistance reported amongst certain species from other countries and increasing Carbapenem resistance seen in our hospital, there is a need to understand the local epidemiology and antimicrobial susceptibility patterns for empirical therapy and drug resistance monitoring.
There is no published data on the epidemiology and resistance rates of Nocardia spp.in living donor related Renal Transplant Recipients from Pakistan. This study aimed to investigate the species distribution, antimicrobial susceptibility and treatment outcomes of clinical Nocardia spp. isolated from renal transplant recipients referred to a tertiary hospital in Karachi, Pakistan.
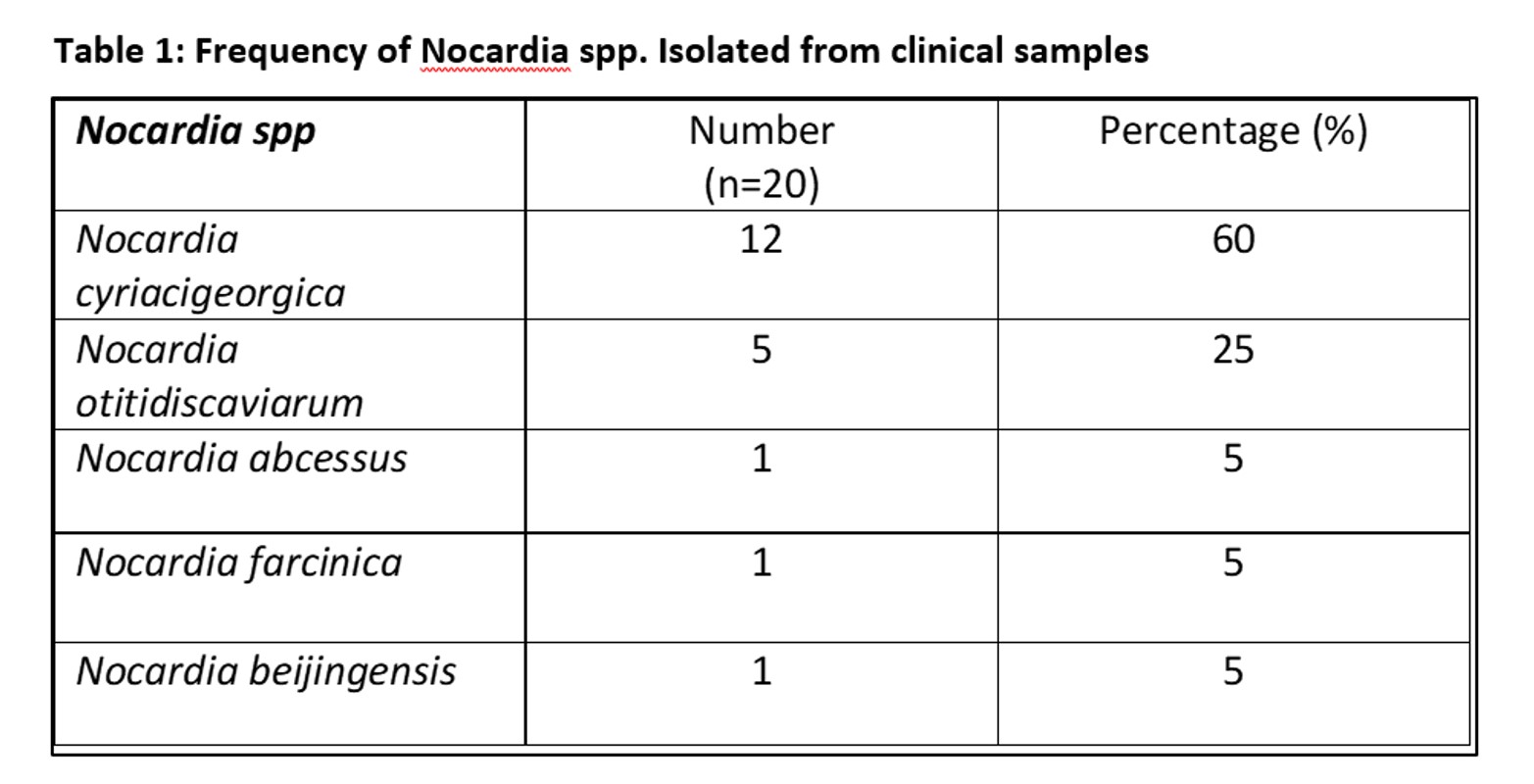
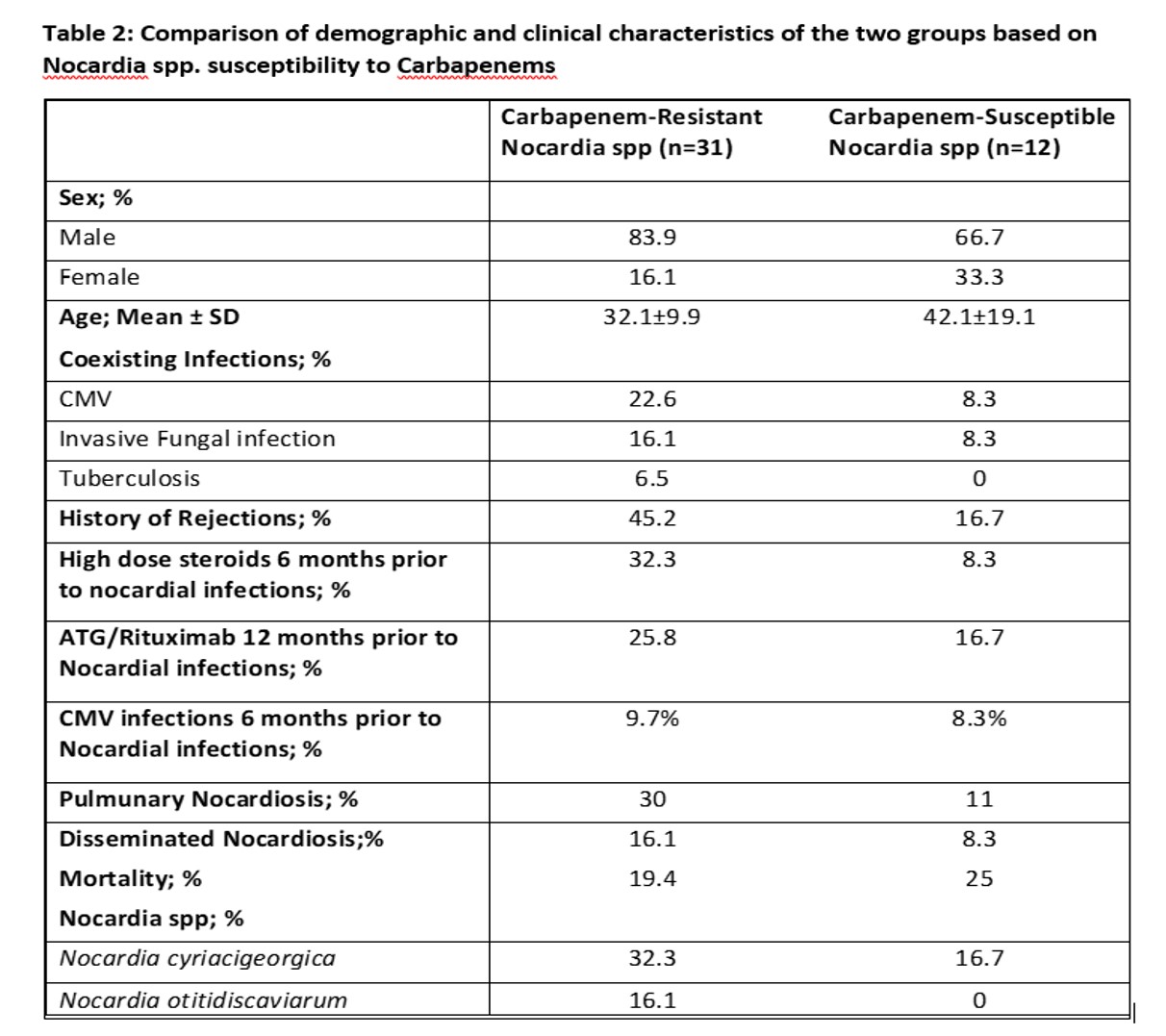
Methods: A total of 43 Nocardia spp. Isolates between 2019 and 2023 from renal transplant recipients were included in the study. Out of 43, 20 isolates were identified to species level by 16S Ribosomal RNA based sequencing. Antimicrobial susceptibility testing was performed for all the isolates using a Sensititre™ RAPMYCOI panel. We also divided our patients into two groups based on Carbapenem susceptibility (Table 2) and compared their Clinical and treatment outcomes. To analyse treatment outcomes, patients with Nocardia infections were followed for 6 months in isolated pulmonary infection and 12 months for disseminated infection.
Results: In this study period, 43 patients were diagnosed with Nocardia infection with a mean age of 34.8±13.6 years. No patients developed Nocardia infection on Cotrimoxazole prophylaxis given for protection of Pneumocystis jirovecci pneumonia. Coinfections with CMV, invasive fungal and TB were seen in 18.6%, 14% and 4.7% patients respectively. At least one rejection episode occurred in 18.6% patients prior to Nocardia infection. The mean time of Nocardia infection after transplant was 5.8±4.1 years. Disseminated infections were seen in 14% of patients. Of the tested isolates, 97.7% displayed susceptibility to Co tromoxazole, Amikacin and Linezolid (Fig.1). In this study, Nocardia cyriacigeorgica was the most frequently isolated Nocardia spp. (n = 12; 60%) (Table 1) with a high Imipenem resistance (Fig.1). Comparing the two groups, there were more coexisting CMV infections, prior Rejections and disseminated Nocardia infections seen in Carbapenem-Resistant Nocardia (Table 2). Mortality was relatively lower in Carbapenem-Resistant group (Table 2).
Conclusion: Nocardia cyriacigeorgica was the most frequently isolated Nocardia spp. and showed high Imipenem resistance. Cotrimoxazole, Linezolid and Amikacin remain good empirical options for treatment of Nocardiosis.
[1] Nocardiosis
[2] Living-Related-Donor
[3] Kidney Transplant
