Public insurance linked to higher graft failure in Hispanic kidney transplant patients: Insights from the 2015-2019 UNOS database
Oscar Garcia Valencia1, Charat Thongprayoon1, Caroline Jadlowiec2, Iasmina Craici1, Shennen Mao3, Napat Leeaphorn3, Pooja Budhiraja2, Wisit Cheungpasitporn1.
1Mayo Clinic, Rochester, MN, United States; 2Mayo Clinic, Phoenix, MN, United States; 3Mayo Clinic, Jacksonville, FL, United States
Introduction: Hispanic kidney transplant recipients encounter disparities impacting their access to care and influence transplant outcomes, such as prolonged waitlist durations and reduced rates of living donor transplantation. Despite demonstrating comparable graft and patient survival rates to non-Hispanic white counterparts, outcomes within the Hispanic population remain markedly heterogeneous. Given the potential significance of insurance coverage in determining access to transplantation and subsequent post-transplantation outcomes, there is a crucial need for focused investigation into its impact within this group.
Methods: Utilizing data from the OPTN/UNOS database spanning 2015 to 2019, we identified Hispanic kidney transplant recipients in the United States. Patients were stratified based on their insurance status, distinguishing between those with public and non-public insurance. Our analysis used Cox proportional hazard analysis to assess death and death-censored graft failure, along with logistic regression analysis to evaluate acute rejection rates among both groups.
Results: Among the 14,639 Hispanic kidney transplant recipients during the study period, 74% (n=10761) were covered by public insurance. Notably, recipients with public insurance tended to be older and presented with higher incidences of diabetes and peripheral vascular disease. Furthermore, they had lower Karnofsky Performance scores, income levels, and education levels. This group also experienced a higher frequency of kidney retransplants, longer durations of dialysis, and fewer preemptive transplants. Additionally, they received kidneys from deceased donors characterized by higher Kidney Donor Profile Index scores and longer cold ischemia times. Importantly, the group with public insurance demonstrated higher 3-year mortality (6.5% vs. 2.8%, p<0.001) and death-censored graft failure rates (6.2% vs. 3.9%, p<0.001) compared to their non-public insurance counterparts. However, upon adjusted analysis, public insurance emerged as a significant predictor of death-censored graft failure (HR 1.38; 95% CI 1.05-1.81) but not patient mortality (HR 1.00; 95% CI 0.76-1.33).
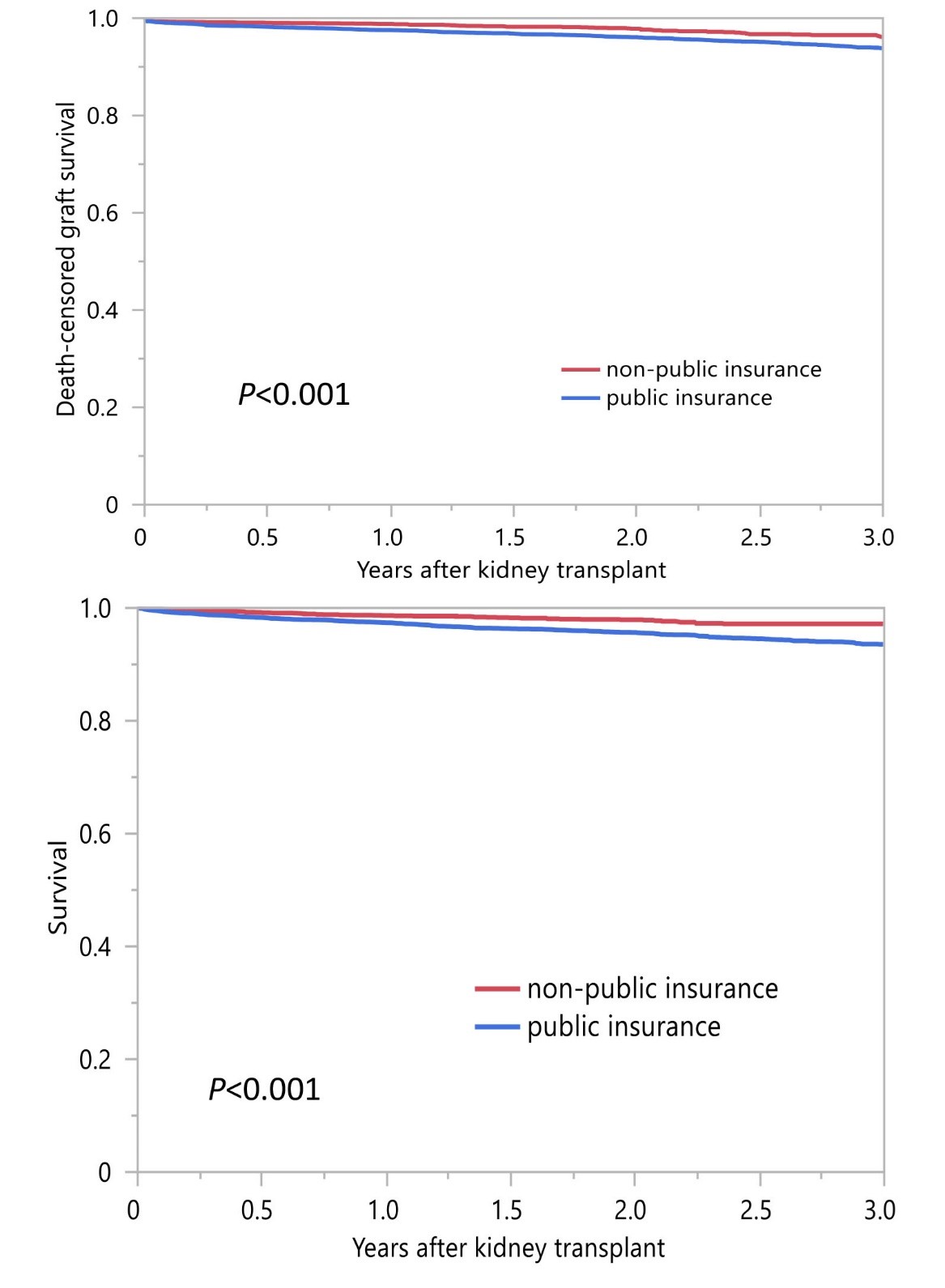
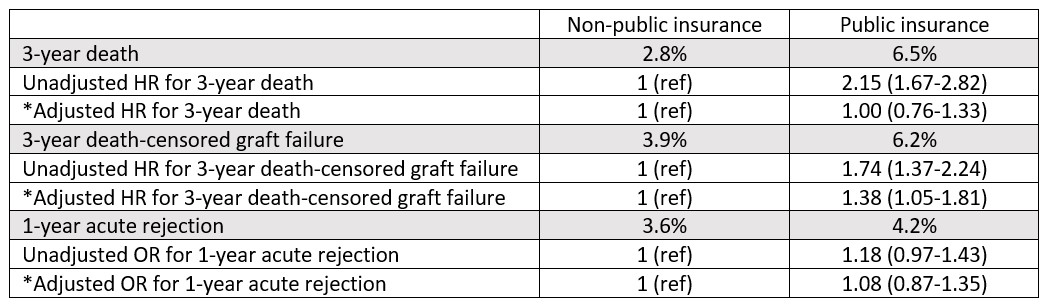
Conclusion: Our study underscores the presence of disparities in post-transplant outcomes among Hispanic recipients, particularly concerning insurance coverage. Public insurance represents a notable predictor of death-censored graft failure, highlighting the necessity for targeted interventions aimed at mitigating these disparities within the Hispanic kidney transplant population.
[1] Healthcare disparities
[2] Public policies
[3] Public insurance
[4] Socioeconomic status
[5] Hispanic Patients
