The respiratory physiotherapy, new use of an old tool to increase lung donor pool
Alberto Sandiumenge1,2, Gonzalo Ballesteros6, Belen Garces5, Joan Marcobal8, Gerard Sanchez-Etayo3, Daniel Marti7, Eduardo Miñambres4, Angela Suarez9, Elisabeth Navas1,2, Irene Bello1.
1Donation and Trasplantation Program Coordination Department, University Hospital Vall d'Hebron, Barcelona, Spain; 2Department of Thoracic Surgery, Respiratory Institute, Hospital Clinic, Barcelona, Spain; 3Department of Donor and Transplant Coordination, Hospital Clinic, Barcelona, Spain; 4Department of Donor and Transplant Coordination, University Hospital Marques de Valdecilla, Santander, Spain; 5Department of Donor and Transplant Coordination, Univeristy Hospital Germans Trias i Pujol, Badalona, Spain; 6Physiotherapy and ocupational therapy Unit. Rehabilitation Department, Unversity Hospital Vall d'Hebron , Barcelona, Spain; 7Rehabilitation and Physiotherapy Department, Hospital Clinic, Barcelona, Spain; 8Rehabilitation and Physiotherapy Departmente, Unversity Hospital Germans Trias i Pujol, Badalona, Spain; 9Rehabilitation and Physiotherapy Department, University Hospital Marques de Valdecilla, Santander, Spain; 10Cell, Tissue and Organ Donation and Trasplantation Group, Vall Hebron Research Institute (VHIR), Barcelona, Spain
Introduction: Mechanical Insufflation-Exsufflation (MI-E) is a non-invasive respiratory physiotherapy device that simulates a cough, aiding in the clearance of secretions and improving oxygenation. Although routinely used for respiratory physiotherapy in critically ill patients, no evidence is available regarding its use in the maintenance/optimization of solid organ donors. We aimed to evaluate the impact on oxygenation, lung compliance and safety when used as a part of the donor management protocol.
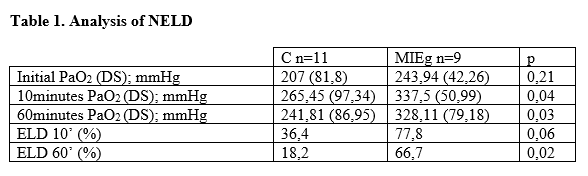
Materials and Methods: A prospective multicenter randomized study was conducted in 4 Spanish centers.. After undergoing a standardized maintenance procedure (OPT) according to Spanish national guidelines, patients were randomized to the control (C) or the interventional group (MIEg- four series of 5 MI-E cycles +40/-60 inspiratory/expiratory pressure-using Cough Assist®). A blood gas analysis (FiO2 1/PEEP 5 mmHg) was obtained before and after OPT, as well as 10 and 60 minutes after MIE (MIEg) or 60 minutes after OPT (C). The study measured PaO2 values, the percentage of gasometrical eligible lung donors (ELD, defined as PaO2/FiO2 > 300 mmHg), and the presence of complications such as pneumothorax or hemodynamic instability resulting from the technique. A sub-analysis of those deemed non-eligible lung donors (NELD- Pa02/Fi02<300mmHg at initial assessment) was performed.
Results: Seventy-one eligible consenting donors were included of whom 20 were considered NELD (28.2%)-Table 1-. Those NELD in the MIEg showed a significant increase in PaO2/Fi02 at 10 and 60 min post-intervention. MIE implementation improved the PaO2 values at 10 and 60 min after intervention increasing the percentage of ELD donors when compared with the control group, No complications derived from the technique were observed.
Conclusion: Respiratory physiotherapy using MI-E is a cost-effective and safe tool to increase the lung donor pool and optimize the donors’ oxygenation. Routine inclusion of MI-E in lung donor management could be considered.
This work has been made with the economical support of Fundación Invest. Médica Mutua Madrileña AP176932021 and Instituto de Salud Carlos III PI21/01911. This work has been presented for its evaluation at the ISHLT 44TH Annual Meeting (2024).
[1] Physiotherapy
[2] Organ donation
[3] Donor Mantainance
[4] lung transplantation
