
Benefit of hypothermic perfusion on kidney graft survival while adding cold ischemia time
Angelica Perez-Gutierrez1, Rita McGill2, Jessica Cao1, Piotr Bachul1, Rolf N Barth1, John Fung1.
1Surgery, University of Chicago , Chicago, IL, United States; 2Medicine, University of Chicago , Chicago, IL, United States
Introduction: Extended cold ischemia time is associated with higher incidence of delayed graft function, primary non-function, and graft failure (1).
Kidneys on hypothermic perfusion have better performance than similar kidneys on ice (2), however the benefit of pumping a kidney and adding cold ischemia time versus ice storage with less cold ischemia time remains unclear, as does the question of how long is safe to wait.
Understanding the safety implications of using kidneys with prolonged cold ischemia time is crucial. Especially considering logistical factors, such as the additional time needed for crossmatch; recipient challenges that require selecting a different recipient (Ej. COVID-19), or the preference for performing complicated surgeries during regular daytime hours when more resources are available.
Methods: This is an analysis of deceased kidney transplants performed from 2005 to 2022 from the UNOS database. We excluded multi-organ, re-transplant, en-bloc, pediatric transplants, and patients who received alternative immunosuppression.
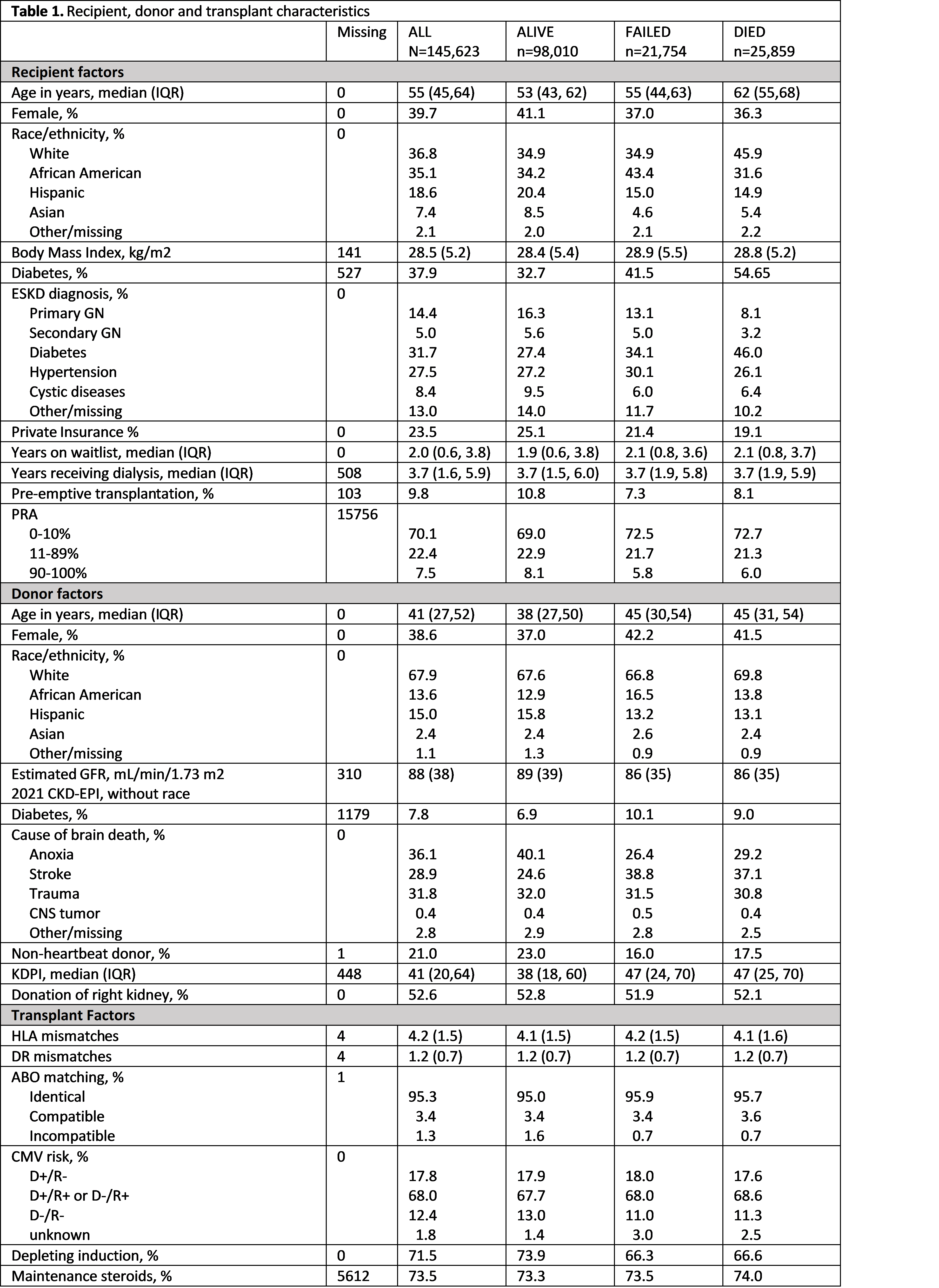
A multivariable Cox model for death-censored graft failure was constructed with 145,623 deceased donor kidney transplants, using kidneys with 11-13 hours on ice as a reference. The model was adjusted for recipient, donor and transplant characteristics shown in Table 1.
Results: A total of 145,623 transplant cases were analyzed. The median cold ischemia time was 18 +/- 9 hrs. 30.9% of the cases were pumped and sent on pump, 51.8% were stored on ice, and 17.3% were pumped and sent on ice. The median of graft survival follow up was 3.9 years (min 1.6, max 7). Table 1 shows the distribution of the recipient, donor and transplant characterisitcs by surival outcome.
Kidneys on hypothermic perfusion have better graft survival than their contra parts on ice with the same CIT. Kidneys with 24 to 36 hours of CIT showed similar censored death graft survival than a reference kidney on ice for ~ 12 hours (HR 1 95% CI 0.93,1.07). Figure 1 shows the hazard ratio of death censored graft failure for kidneys on ice or pump compared to a reference kidney on ~12 hours on ice.
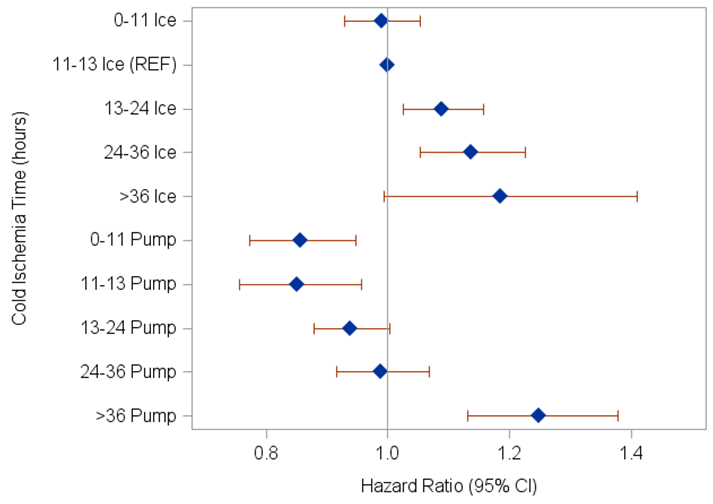
Kidneys with CIT > 36 hours have higher incidence of death censored graft failure regardless of the storage method.
Conclusions: Hypothermic perfusion is an effective strategy for mitigating the effects of prolonged CIT, thus providing greater flexibility in donor and recipient logistics. Prolonged CIT on pump, up to 36 hours has equivalent graft survival than kidneys with less than 12 hours on ice.
References
1. Lum EL, Homkrailas P, Abdalla B, et al. Cold Ischemia Time, Kidney Donor Profile Index, and Kidney Transplant Outcomes: A Cohort Study. Kidney Med. 2022;5(1).
2. Moers C, Smits JM, Maathuis MH, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2009;360(1):7-19.
[1] cold ischemia time
[2] hypothermic perfusion
[3] kidney transplant
