Impact of hypothermic machine perfusion on delayed graft function in kidney pairs from the same deceased donor in the United States
Mohammed Mahgoub1, Ahmed Z Alrifai1, Amanda L Tapia2, Byron Smith2, Naim Issa1, Hatem Amer1, Patrick Dean3, Samy Riad1.
1Nephrology and Hypertension, Mayo Clinic Transplant Center, Rochester, MN, United States; 2Clinical Trials and Biostatistics, Mayo Clinic Transplant Center, Rochester, MN, United States; 3Division of Transplantation Surgery, Mayo Clinic Transplant Center, Rochester, MN, United States
Background: Delayed graft function (DGF) is a common early challenge in kidney transplantation linked to adverse short- and long-term outcomes. This study investigates the association between hypothermic machine perfusion and delayed graft function in recipients of kidney pairs from the same donor.
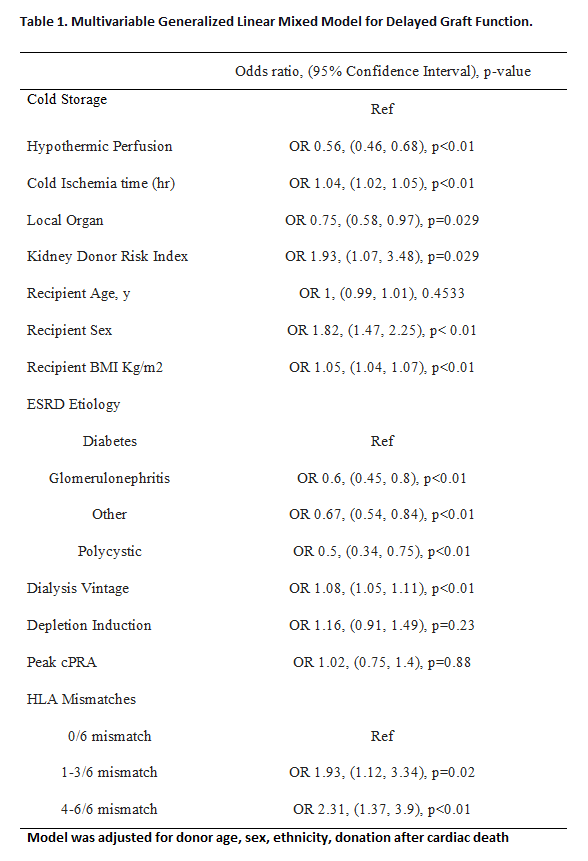
Methods: Utilizing the Scientific Registry of Transplant Recipients (SRTR), we identified dialysis-dependent primary deceased donor kidney recipients from 2014 to 2022. We excluded recipients with missing or mixed induction and those with positive or unknown crossmatch status. All recipients received an ABO-compatible organ and were discharged on tacrolimus and mycophenolate, with or without prednisone maintenance. The focus was on recipients of kidneys from the same donor, with one kidney undergoing hypothermic machine perfusion before transplantation. Recipients were categorized into two groups: the perfusion group and the cold static storage group. We compared pretransplant variables and posttransplant outcomes between the 2 induction groups with chi square or Wilcoxon tests, as appropriate. A multivariable generalized linear mixed model, adjusted for relevant donor and recipient characteristics, with donor I.D. and the organ procurement organization (OPO) included as random effects, was employed to examine the association between hypothermic machine perfusion and delayed graft functions.
Results: Among 1950 donors contributing 3900 deceased donor kidneys meeting the criteria, hypothermic perfusion was applied to one kidney from each donor. Recipient characteristics, including age, sex, ethnicity, BMI, and vascular comorbidities, were comparable between the groups. Notably, the perfusion group had more recipients with diabetes mellitus (36% vs. 33.3%, p < 0.01) and 4-6 HLA-mismatches (80.8% vs. 76.5%, p < 0.01) compared to the cold static storage group. Cold ischemia time was longer in the perfusion group (20.4 hr vs. 14.7 hr, p < 0.01), while time on dialysis was slightly shorter in the perfusion group recipients (5.0 yr vs. 4.7 yr p<0.01). Induction and steroid maintenance did not differ between groups. In the multivariable model, compared to cold storage, machine perfusion was associated with a 44% reduction in the odds of DGF (OR 0.56, 95% C.I. 0.46-0.68, p < 0.01).
Conclusion: In this distinct cohort of deceased donor kidney pair recipients, machine perfusion significantly reduced the odds of delayed graft function, demonstrating independence from recipient factors or cold ischemia time.
The data reported here have been supplied by the Hennepin Healthcare Research Institute (HHRI) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government..
[1] Delayed graft function
[2] Machine perfusion
[3] Deceased donors kidney pairs
