Early experience with oxygenated hypothermic machine perfusion for kidney transplantation at a single center in the United States
Justin Steggerda1, Irene K Kim1, Tsuyoshi Todo1, Todd V Brennan1, Alice Peng2, Edmund Huang2, Jun Shoji2, Reiad Najjar2, Georgios Voidonikolas1, Steven A Wisel1.
1Transplant Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, United States; 2Transplant Nephrology, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Introduction: Oxygenated hypothermic machine perfusion (HMPO2) represents emerging technology in kidney preservation and has been shown to reduce rates of delayed graft function (DGF) and improve graft function at 6-months following kidney transplantation (KTx). Here we report the early experience of a single, high-volume center in the United States with HMPO2.
Methods: Patients who received kidney allografts which underwent HMPO2 prior to transplantation using Kidney Assist Transport (XVIVO, Molndol, Sweeden) were included. All grafts were received on cold storage and transitioned to HMPO2 at our center. Donor, recipient, and transplant characteristics were analyzed. All patients received standard induction and post-transplant immunosuppression. Early post-operative graft function, DGF (defined as dialysis within first week after transplant), and 30-day graft function are reported.
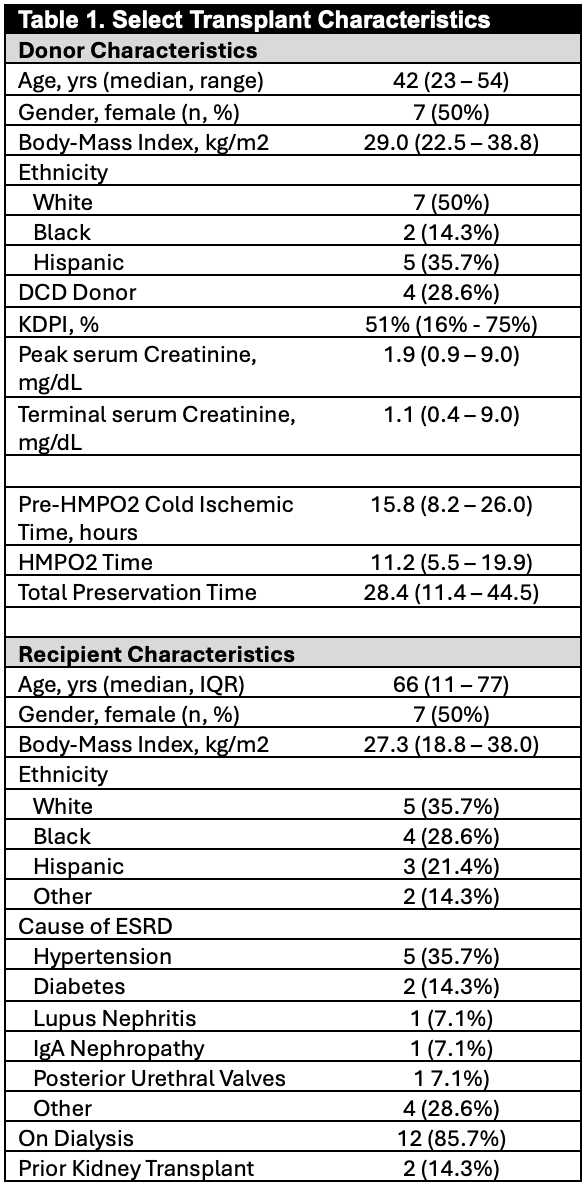
Results: Overall, 14 patients received allografts preserved with HMPO2. Eight kidneys (57.1%) were imported from other organ procurement organizations, and the most common indications for HMPO2 were prolonged cold ischemic time (CIT, n=6, 42.8%), donation after circulatory death (DCD, n=4, 28.6%), and recipient-related issues (n=35.7%). Donor and recipient characteristics are presented in Table 1. Notably, median kidney donor profile index (KDPI) was 51% (range 16%-75%) with 4 (28.6%) being DCD donors and 8 with acute kidney injury (AKI, serum Cr >1.5mg/dL during hospitalization). Median Pre-HMPO2 CIT was 15.8 hours (range 8.2-26.0 hours) and HMPO2 time was 11.2 hours (5.5-18.8 hours), leading to total preservation time of 28.4 hours (18.4-44.5 hours). Despite these long CIT and preservation times, early outcomes showed 10/14 (71.4%) recipients had immediate graft function and all (100%) patients were discharged off dialysis after median post-KTx length of stay of 5 days. Of the 4 patients with DGF, 2 were from the same donor which had terminal serum Cr of 9.0mg/dL and both had their last dialysis on post-operative day 4, and one patient was dialyzed for post-operative hyponatremia in the setting of good urine output. There was no incidence of primary non-function in this group, even with preservation times >40 hours. Two patients had peri-operative complications (1 with sepsis, 1 with post-op bleeding) which were managed with preserved graft function. 30-day follow-up was available for 8 patients with median estimated glomerular filtration rate (eGFR) of 43ml/min and no episodes of rejection observed.
Conclusions: The early experience at our center shows that while taking kidneys from marginal donors (i.e., AKI, DCD), kidneys from distant donors with long CIT, and overcoming recipient and logistical issues. We found decreased DGF rates of 28% compared to >50% historically for similar cohort at our institution, with excellent early graft function and no patients requiring routine dialysis after discharge.
[1] Kidney Transplant
[2] Donation After Circulatory Death
[3] Marginal Kidney
[4] Delayed Graft Function
[5] Organ Preservation
