Regional disparities in kidney transplant allocation in Brazil
Daniela F Salomao1,2, Luis Gustavo M de Andrade1,2, Gustavo F Ferreira2, Abner MP Barbosa1, Naila C da Rocha 1.
1Fisiopatologia, UNESP, Botucatu, Brazil; 2Coordenacao EM Transplante, ABTO, Sao Paulo, Brazil
Introduction: Brazil has a large Public Transplant Program, but I It remains unclear if the kidney allocation criteria is effective. This study aimed to investigate whether gender, ethnicity, clinical characteristics, and Brazilian regions affect the likelihood of receiving a transplant.
Methods: We conducted a retrospective cohort study using the National Transplant System/Brazil database, which included all patients on the kidney transplant waitlist from January 2012 to December 2022, followed until May 2023. The primary outcome assessed was the likelihood of kidney transplantation with a deceased donor, measured using the hazard ratio (HR).
Results: We analyzed 118,617 waitlisted patients over 10-year study period. The median age at waitlist entry was 48 years (IQR: 37-58), with 60% being male. The majority were Caucasian (51%), followed by mixed race (48%). Most patients were from the Southeast region (54%), while the minority were from the North region (5.2%).
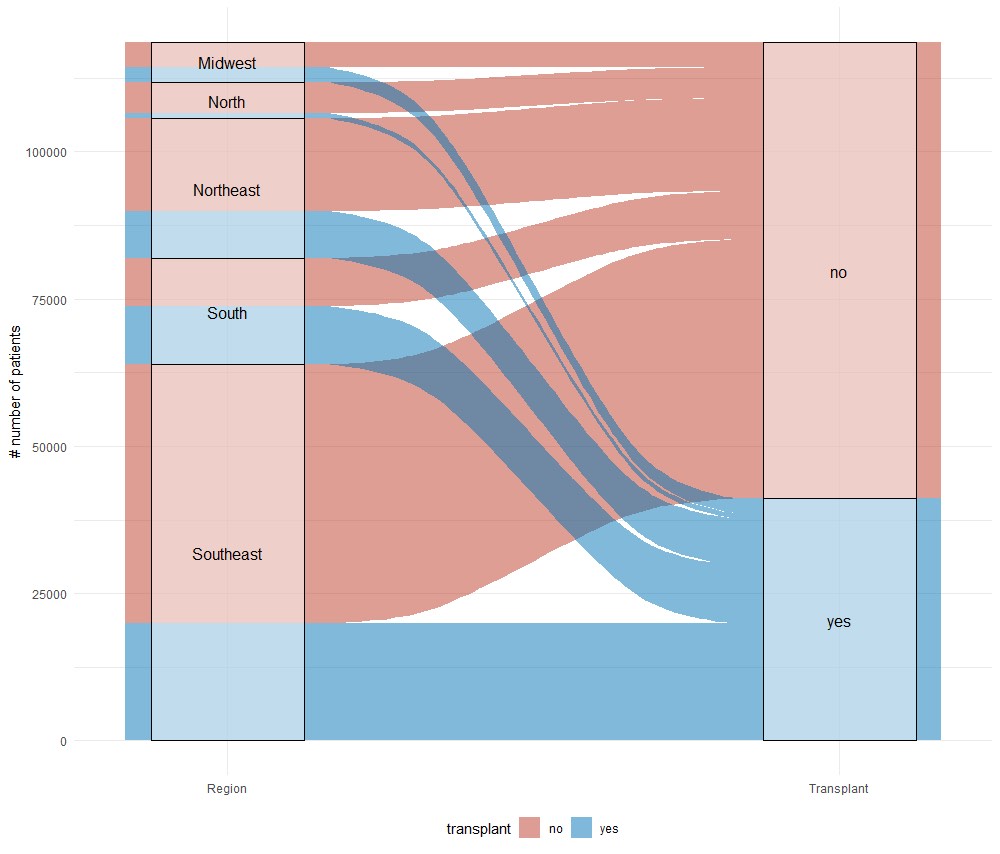
The majority had blood type O (50%) and a cPRA of zero (67%). During the period, 41,111 patients were transplanted (35%), with a median time to transplantation of 17 months (IQR: 9-33), and 11,911 (10%) died on the waitlist. Male patients had a 1.07 [95% CI: 1.05 – 1.10], p < 0.001 higher probability of receiving a transplant. Patients of mixed race and Yellow/Indigenous ethnicity had lower probabilities of receiving a transplant compared to Caucasian patients, with probabilities of 0.97 [95% CI: 0.95 – 1] and 0.89 [95% CI: 0.95 – 1], respectively. Patients from the South region had the highest probability of receiving a transplant, followed by those from the Midwest and Northeast, compared to patients from the Southeast, with probabilities of 2.53 [95% CI: 2.47 – 2.61], 1.21 [95% CI: 1.16 – 1.27], and 1.10 [95% CI: 1.07 – 1.13], respectively. The North region had the lowest probability of receiving a transplant, at 0.29 [95% CI: 0.27 – 0.31].
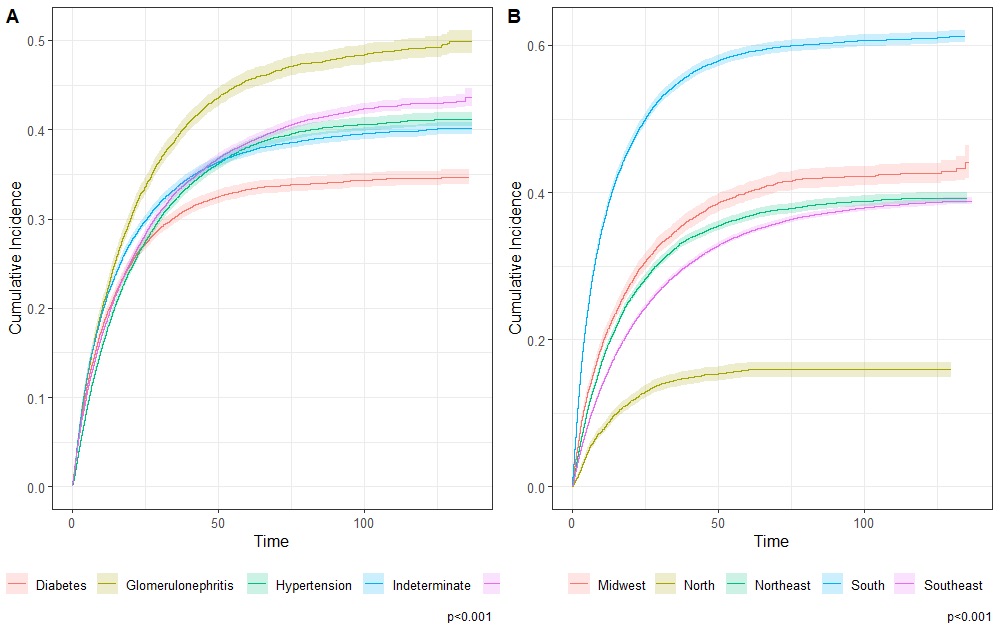
The highest number of patients on the waitlist were concentrated in the Southeast (n=63,855, 53.8%), followed by the South (n=18,057, 15.2%) and Northeast regions (n=23,733, 20%), Figure 02. Patients from the South and Southeast region had better access to the transplant list, being on dialysis for 12 (5,28); and 12 (6,27) months followed by those from the Midwest 21 (10,46), North 23 (10,54) and Northeast 25 (12,56), respectively.
Conclusion: We found that women and racial minorities faced disadvantages in kidney transplantation. Additionally, we observed regional disparities, with the North region having the lowest probability of receiving a transplant and longer times on dialysis before being waitlisted. In contrast, patients in the South regions had a higher likelihood of receiving a transplant and shorter times on dialysis before being waitlisted. It is urgent to implement approaches to enhance transplant capacity in the North region and address race and gender disparities in transplantation.
