Clinical significance of grade A small-for-size syndrome after living-donor liver transplantation utilizing the new definition of diagnostic criteria: An international multicenter study
Dong-Sik Kim1, Hye-Sung Jo1, Vasanthakumar Gunasekaran2, Jagadeesh Krishnamurthy3, Takeo Toshima4, Ryugen Takahashi5, Jae-Yoon Kim6, Sathish Kumar Krishnan7, Shinya Okumura8, Takanobu Hara9, Keita Shimata10, Koichiro Haruki11, Robert C. Minnee12, Ashwin Rammohan2, Subash Gupta3, Tomoharu Yoshizumi4, Toru Ikegami11, Kwang-Woong Lee6, Mohamed Rela2.
1Surgery, Korea University College of Medicine, Seoul, Korea; 2Liver Disease & Transplantation, Dr.Rela Institute & Medical Centre, Chennai, India; 3Liver Transplant and HPB Surgery, Max Super Speciality Hospital, Saket, India; 4Surgery and Science, Kyushu University Hospital, Kyushu , India; 5Surgery, University of Tokyo, Tokyo, Japan; 6Surgery, Seoul National University Hospital, Seoul, Korea; 7HPB and Liver Transplantation, Gleneagles Global Hospital, Chennai, India; 8Surgery, Kyoto University, Kyoto, Korea; 9Surgery, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan; 10Pediatric Surgery and Transplantation, Kumamoto University Hospital, Kumamoto, Japan; 11Surgery, The Jikei University School of Medicine, Tokyo, Japan; 12Surgery, Erasmus Medical Center, Rotterdam, Netherlands
International Living Donor Liver Transplantation Group.
Introduction: New diagnostic criteria have recently been established to classify small-for-size syndrome (SFSS) after living-donor liver transplantation (LDLT) into three groups based on severity; however, its clinical significance needs to be validated. This study aimed to evaluate the clinical impact of grade A SFSS and identify the risk factors for survival through subgroup analysis.
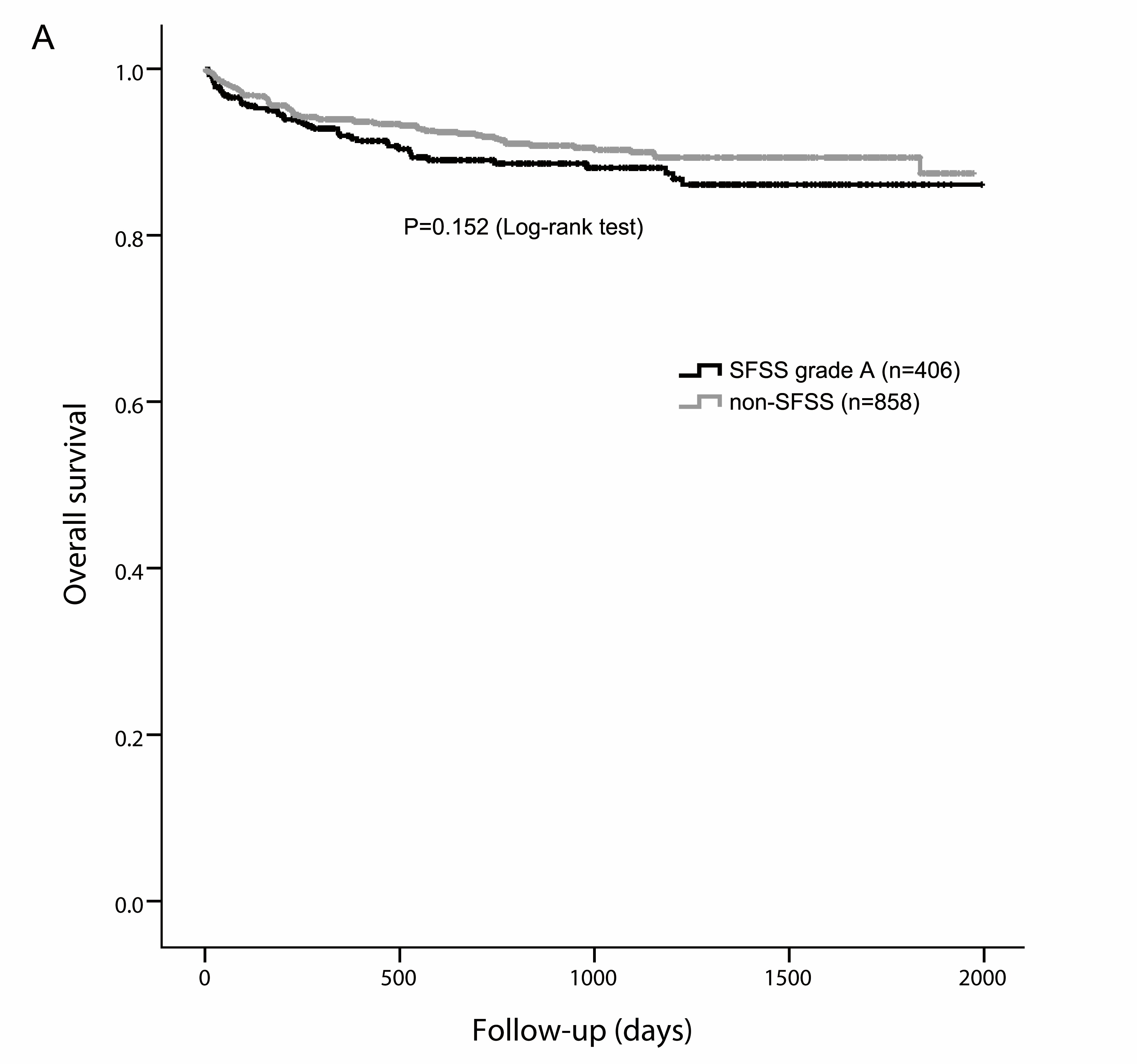
Method: We collected data from 406 patients diagnosed with grade A SFSS after LDLT between 2018 and 2022 at 12 hospitals of the International Living Donor Liver Transplantation Group. Survival data were collected from 858 patients without SFSS. After exclusion, the final cohort consisted of 363 patients. We categorized 55 (15.2%) in the uptrend group, 251 (69.1%) in the downtrend group, and 57 (15.7%) in the ascites group according to the level and trend of total bilirubin on postoperative days 7 and 14.
Results: There was no significant difference in survival between patients with and without grade A SFSS (P=0.152).
In the subgroup analysis, the graft-to-recipient body weight ratios (GRWRs) were comparable between the up-trend, down-trend, and ascites groups (P=0.168). The uptrend group showed higher 30-day and 90-day mortality rates than the downtrend and ascites groups (P=0.076 and P=0.030, respectively). The 1-year survival rate differed significantly between the groups (88.8%, 93.1%, and 98.2%, respectively; P=0.005).
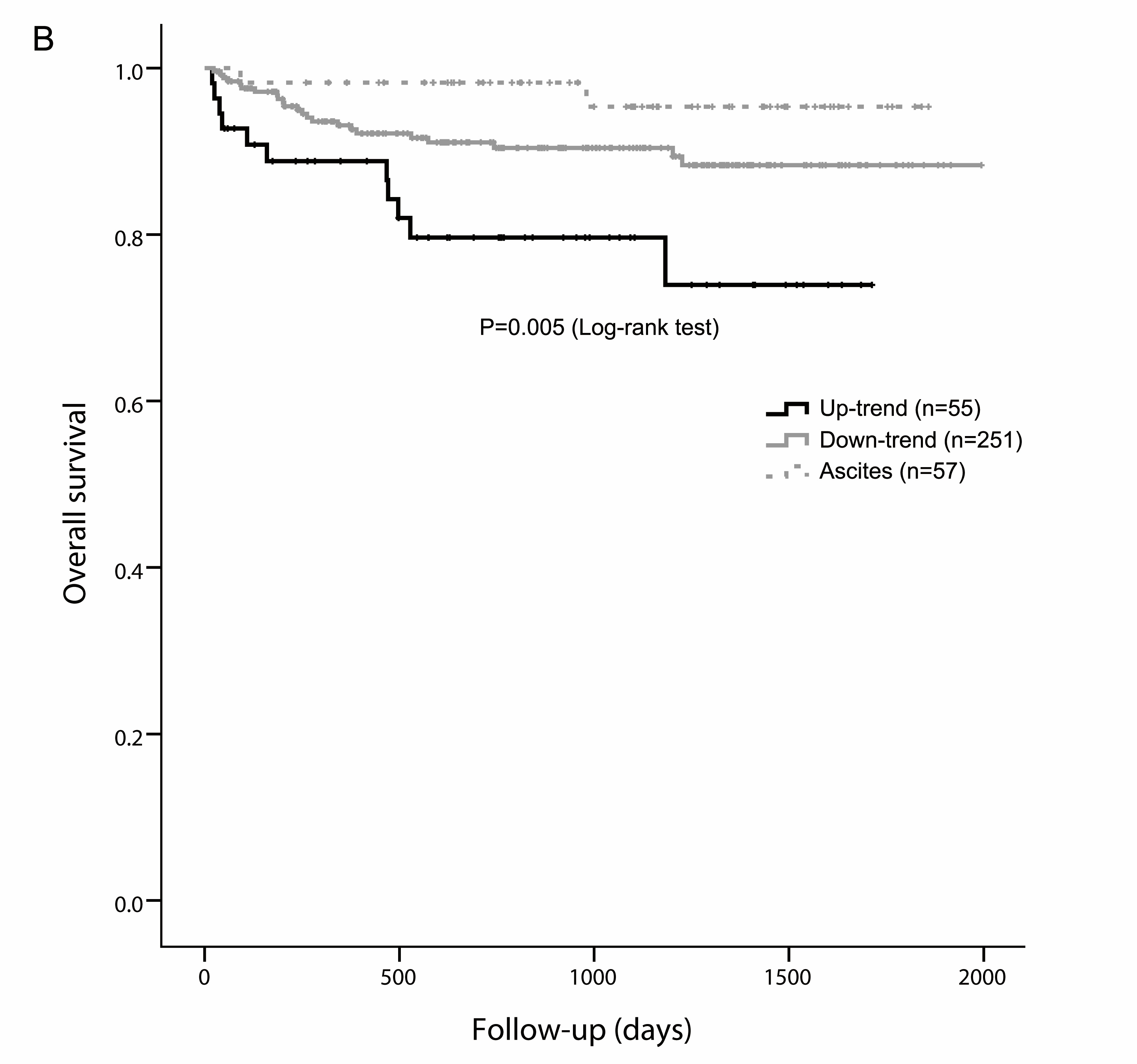
The independent risk factors for survival were up-trend of total bilirubin, recipient age (≥65), MELD score (≥30), and ABO incompatibility. Patients with two or more risk factors had worse survival rates than those with none and only one risk factor (P<0.001).
Conclusion: Although the overall survival rate was comparable between patients with and without grade A SFSS, the uptrend group showed worse short- and long-term outcomes. Aggressive interventions, such as portal inflow modulation, should be considered for up-trend patients with risk factors.
