Factors influencing the use of non-ideal deceased donor livers for transplantation: A qualitative study of U.S. transplant center leaders
David Cron1,2, Rafal D Mazur3, Kristen Kennefick4, Joel Adler5, Keren Ladin4,6, Heidi Yeh1.
1Surgery, Massachusetts General Hospital, Boston, MA, United States; 2Center for Surgery and Public Health, Brigham and Women's Hospital, Boston, MA, United States; 3Harvard Medical School, Boston, MA, United States; 4Research on Ethics, Aging, and Community Health (REACH Lab), Medford, MA, United States; 5Surgery and Perioperative Care, University of Texas at Austin, Austin, TX, United States; 6Community Health, Tufts University, Medford, MA, United States
Introduction: Despite the shortage of donor livers available for transplant, ten percent of available deceased-donor livers go unused in the U.S. Non-ideal donor livers (NIDLs)—e.g. donation after circulatory death, steatotic, or older donors—are organs previously associated with inferior outcomes, but more recently with acceptable outcomes. Transplant centers vary in their utilization of NIDLs, and the factors underlying this variation are unclear. We interviewed US transplant center leaders to identify facilitators and barriers to the use of NIDLs for transplant and to identify strategies to improve utilization.
Methods: We conducted semi-structured interviews with liver transplant surgical leaders in 19 US transplant centers across 10 OPTN regions. We applied purposive sampling criteria to recruit both high/low NIDL utilizers within each region. A codebook was developed through a combination of deductive/inductive approaches, allowing new codes to emerge. Interview recordings were transcribed, de-identified, and coded by two coders. Guided by an ecological model of the transplant system, we employed thematic analysis to uncover emerging themes related to transplant centers’ approach to NIDLs and identified facilitators and barriers to using more NIDLs. We also compiled strategies for improving the use of NIDLs nationally as recommended by the participants.
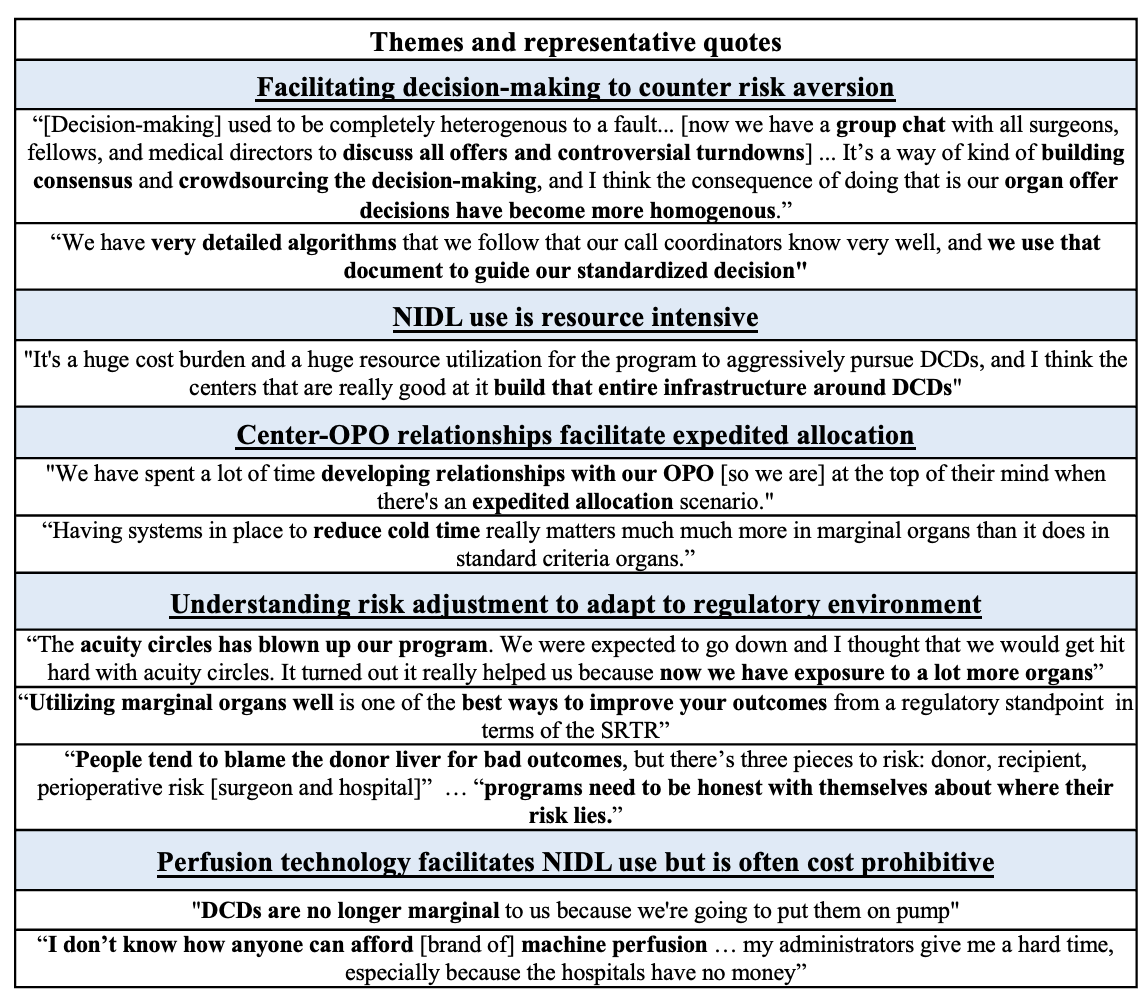
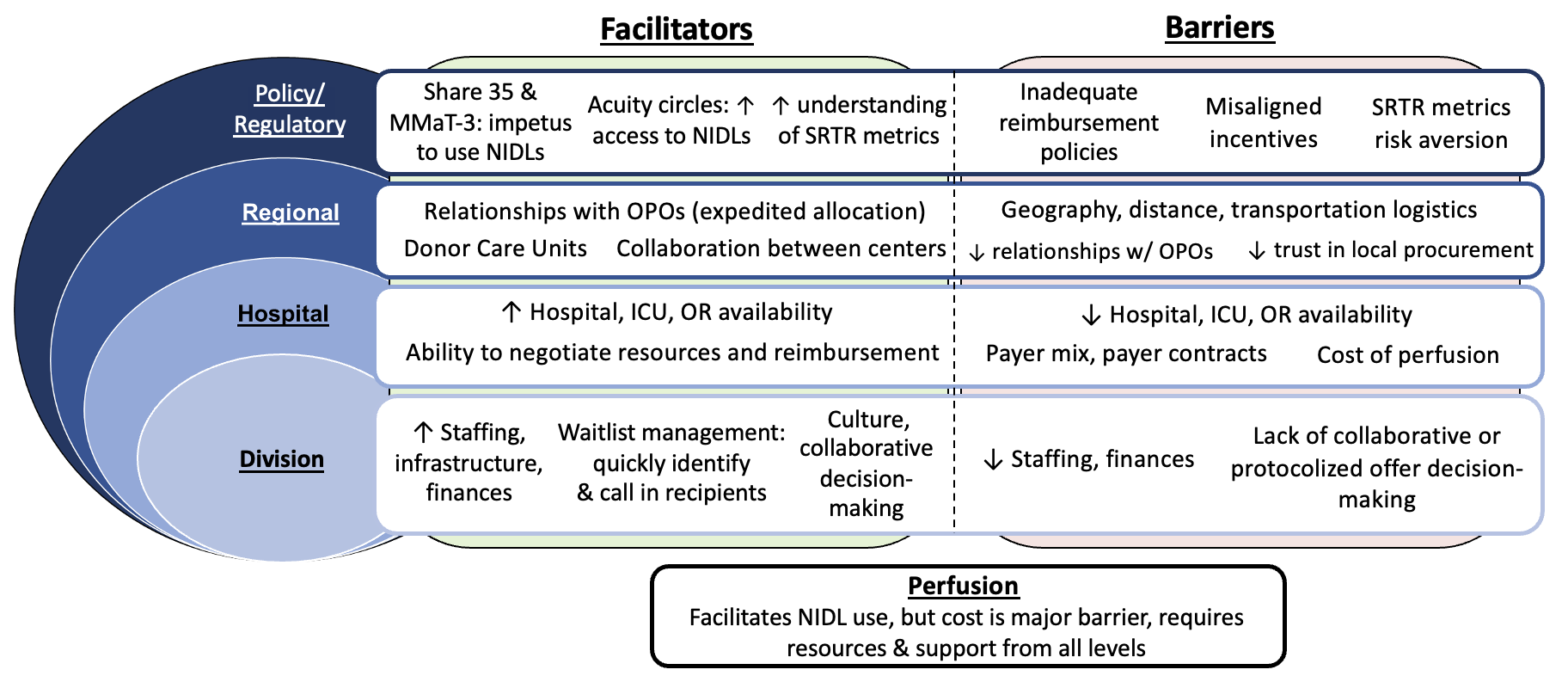
Results: Five themes emerged related to how centers approach NIDLs (Figure 1). 1) Facilitating decision-making to counter risk aversion. 2) NIDL use is resource intensive. 3) Center-OPO relationships facilitate expedited allocation. 4) Understanding risk adjustment to adapt to regulatory environment. 5) Perfusion technology facilitates NIDL use but is often cost prohibitive. Figure 2 shows barriers and facilitators to NIDL use across levels of the transplant ecosystem. Interviewees proposed potential strategies to improve NIDL use nationally: enhanced collaboration and best practice sharing, greater understanding of viability assessment with perfusion, increased reimbursement for perfusion and NIDLs, and refined policies to facilitate expedited allocation of NIDLs.
Conclusion: The determinants of NIDL use are multifactorial and span all levels of the transplant ecosystem. These findings may elucidate areas of intervention or process improvement for transplant centers seeking to increase their NIDL utilization. Policies around reimbursement, organ allocation, and performance metrics should consider their effect on NIDL utilization.
[1] deceased donor
[2] liver transplant
[3] donor selection
[4] candidate selection
[5] DCD
[6] perfusion
[7] decision making
[8] transplant center
