Consultant Transplant Surgeon - Kidney, Pancreas and Intestinal Transplant
Incidence of malignancy after intestinal transplant
Mahesh Polamreddy1, Charlotte Yates2, Pedro Simas2, Charlotte Rutter1, Srikanth Reddy2, Philip Allan2, Andrew Butler1, Neil Russell1, Irum Amin1, Emilio Canovai2.
1Cambridge Centre for Intestinal Rehabilitation and Transplant (CamCIRT), Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom; 2Oxford Transplant Centre, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Introduction: All transplants are associated with an increased lifetime risk of malignancy due to immunosuppression. Given the higher level of immunosuppression in intestinal transplant (ITx), there is a concern this risk may be considerably higher in this group of patients. In kidney transplant recipients this risk has shown to be three times higher than a baseline population in the recipient’s lifetime, but the risk of de novo malignancy has never been quantified after ITx.
Method: A retrospective study was conducted from both centres performing adult ITx in the United Kingdom. Records from intestinal transplant recipients from 01/01/2015 to 01/04/2024 were reviewed to ascertain the occurrence of transplant de novo malignancies. Post-transplant lymphoproliferative disorder (PTLD) and patients who had progression of their primary malignancy were excluded in the final analysis.
Results: 140 ITx were performed across both sites in this period. The mean age of recipients was 44.5. Distribution of ITx types were: 53% isolated small bowel, 18% liver-small bowel, 12% modified multivisceral, 17% multivisceral. Indications were loss of vascular access, liver disease, Porto mesenteric thrombosis and re-transplantation.
Of these, 18 patients developed 25 malignancies. The main categories were skin (33%), cervical (12%), haematological (8%), lung (8%) and gastric (8%). The distribution of these malignancies can be seen in Figure 1. Out of ITx patients who developed de novo malignancies 17% also developed PTLD. The mean age of diagnosis was 54 years. There was a 61% incidence of previous smoking in the group, although no one was a current smoker. The 5-year survival rate of the 18 patients was 33% compared to the overall published 5-year survival rate in the UK post intestinal transplant of 62%. The malignancy was the cause of death for 55% (n=10) of the 18 patients.
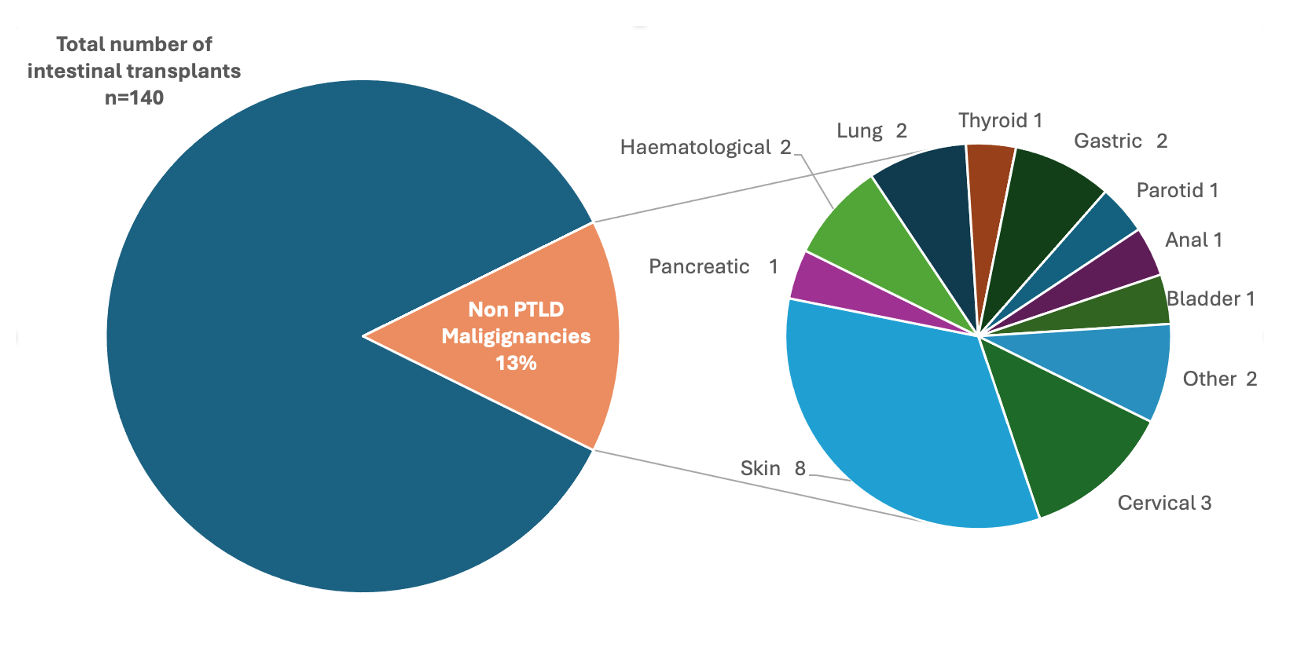
Conclusion: From analysing retrospective data of all adult intestinal transplant patients, the rate of non-PTLD malignancy is 13% post ITx transplant. This rate of de novo malignancy and subsequent poor outcomes should prompt careful counselling. Harm reduction such as UV protection, smoking cessation and regular follow-up should be undertaken. Further assessment of risks factors for developing malignancy should be conducted in this patient’s cohort to help further stratify individual risk for developing malignancy.
[1] Intestinal Transplantation
[2] Malignancy
[3] Multivisceral Transplantation
