Association of macrovascular invasion and poor tumor differentiation on post-liver transplant outcomes in patients with hepatocellular carcinoma
Nazli Begum Ozturk1, Merve Gurakar2, Marwan Alsaqa3, Alan Bonder3, Ahmet Gurakar2, Behnam Saberi3.
1Internal Medicine, Beaumont Hospital, Royal Oak, Royal Oak, MI, United States; 2Gastroenterology and Hepatology, Johns Hopkins University School of Medicine, Baltimore, MD, United States; 3Gastroenterology and Hepatology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, United States
Introduction: Liver transplantation (LT) is one of the main treatment options in selected patients with hepatocellular carcinoma (HCC). The presence of macrovascular invasion is a contraindication to LT due to the high risk of post-LT HCC recurrence. Determination of macrovascular invasion before LT is based on radiological findings; however, liver explant pathology remains the most accurate evaluation for vascular invasion. In this study, we aimed to investigate post-LT outcomes of patients with vascular invasion and tumor differentiation detected on the liver explants in a large national US database.
Methods: LT candidates with HCC between 2012 to 2022 using the UNOS/OPTN database were identified. Patients who underwent deceased donor LT and with liver explant pathology data were included. Kaplan-Meier curves were used for survival analysis. Multistep regression analysis was used to determine the predictors of mortality.
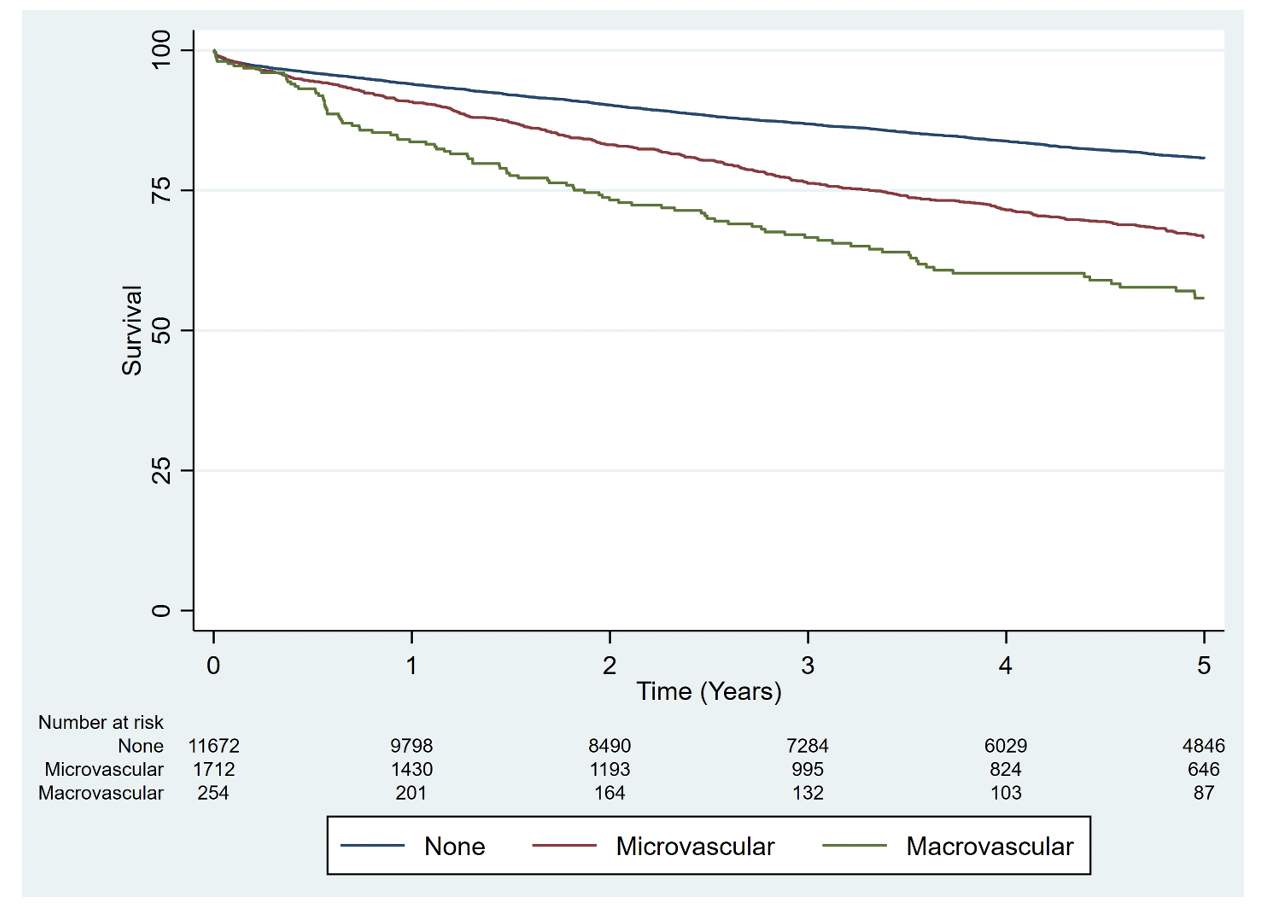
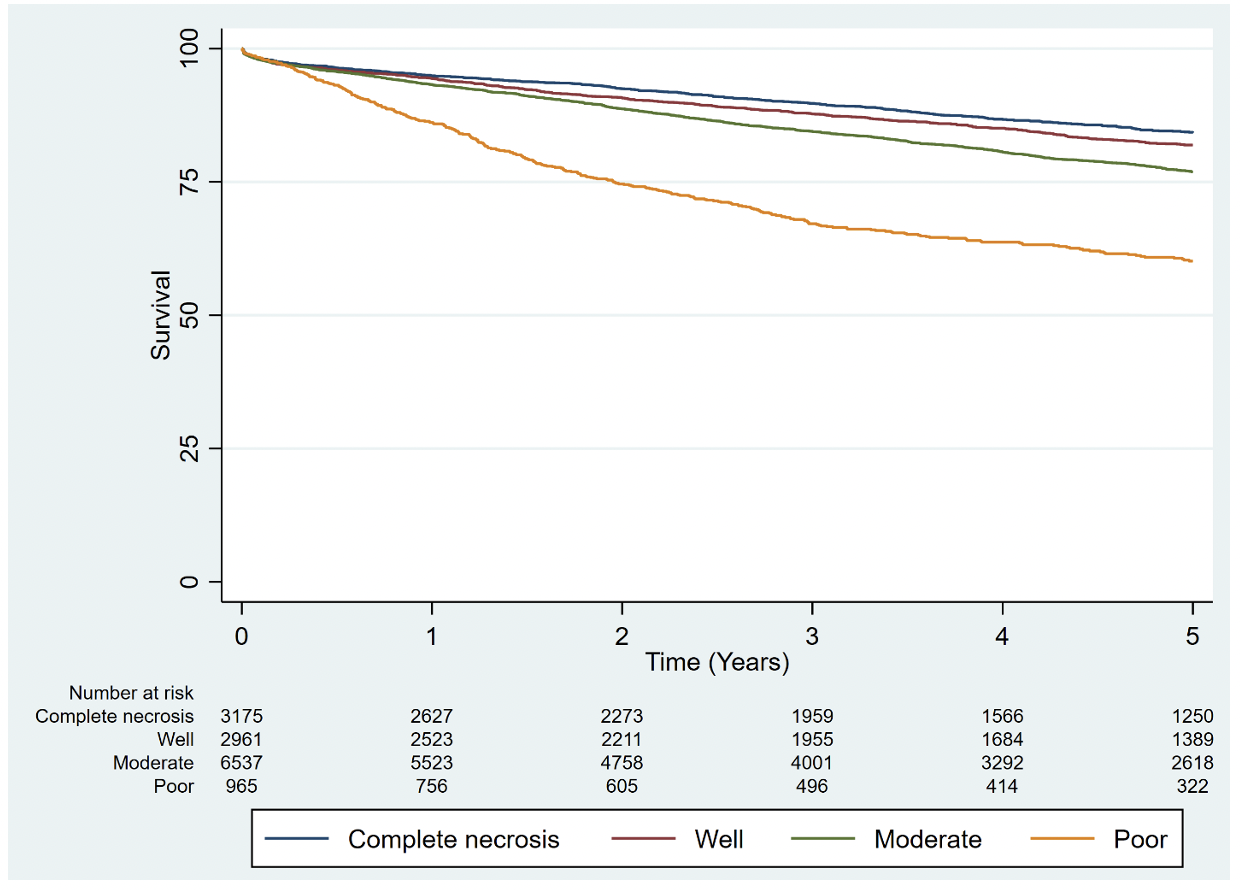
Results: A total of 13,638 patients with HCC and available data on vascular invasion status in liver explants were identified. Among these, 254 (1.8%) had macrovascular invasion, 1712 (12.6%) had microvascular invasion, and 11,672 (85.6%) had no vascular invasion. Poor tumor differentiation was more common in the macrovascular invasion group, compared to microvascular and no-vascular invasion groups (22.4%, 17.7%, and 5.1%, respectively, p<0.001). Patients with macrovascular invasion had a lower 1-, 3-, and 5-year post-LT survival compared to microvascular invasion and no vascular invasion groups (83.6%, 66.6%, 55.7%, and 90.8%, 76.2%, 66.6%, and 93.9%, 86.8%, 80.7%, respectively, p<0.001) (Figure1). Patients with poor tumor differentiation on liver explants had a lower 1-, 3-, and 5-year post-LT survival compared to well-differentiated and complete necrosis on liver explants (86.1%, 67.1%, 60.4%, and 94.3%, 87.7%, 81.9%, and 94.8%, 89.7%, 84.2%, respectively, p<0.001) (Figure2). In multivariate analysis, patients with macrovascular invasion had a higher hazard of mortality compared to those with no vascular invasion (HR=2.269, 95% CI:1.876-2.745). In multivariate analysis, patients with poor tumor differentiation had a higher hazard of mortality compared to complete necrosis on explant (HR=2.332, 95% CI:2.027-2.684).
Conclusion: The presence of macrovascular invasion on liver explants in patients with HCC was associated with worse post-LT survival, with macrovascular invasion being associated with the highest mortality. In addition, tumor differentiation on liver explants was also significantly associated with post-LT survival, in particular in patients with poorly differentiated tumors. Preoperative imaging before LT may not always correlate well with the liver explant pathology and may not detect macrovascular invasions. Explant data have the potential to be incorporated into prognostic scoring systems for post-LT survival.
[1] hepatocellular carcinoma
[2] vascular invasion
[3] tumor differentiation
[4] liver transplantation
