
Living donor liver transplant in Shiraz, Iran; preliminary analyses of a 20-year experience in children and adults
Alireza Shamsaeefar1, Amirali Mashhadiagha1, Nasrin Motazedian1, Kourosh Kazemi1, Hamed Nikoupour1, Seyed Ali Moosavi1, Rozhan Abdollahzade1, Mehrab Sayadi1, Seyed Ali Malek Hosseini1, Saman Nikeghbalian1.
1Shiraz Transplant Research Center, Shiraz University of Medical Sciences , Shiraz, Iran
Introduction: Since its inception in 1989, living donor liver transplantation (LDLT) has sparked controversy due to its dual nature of offering significant benefits such as reduced waitlist and post-transplant mortality rates, as well as decreased post-operative complications for recipients, while also raising health risks for the living donor and ethical concerns in the field of transplantation.
Methods: A retrospective study was conducted on the survival and postoperative complications of LDLT recipients at the Shiraz Transplant Center, Iran's leading liver transplant facility, spanning from 1994 to 2023.
Results: The study included 121 adult recipients (with a mean age of 39.68 years) and 662 pediatric recipients (with a mean age of 5.034 years). In the adult group, autoimmune hepatitis (17.4%) was the primary cause of End-stage Liver disease (ESLD), the right lobe was the most common part harvested (84.3%), and mean MELD score was 18. Infections (58), primary nonfunction (45), and rejection (30) were the most common post-LDLT complications which resulted in 42 adult recipient deaths. Older age, higher BMI, and more frequent post-op convulsion, bleeding, and portal vein thrombosis were found to be more common in the adults’ death group. Mean survival was 7.82 years, and the average follow-up was 4.6 years.
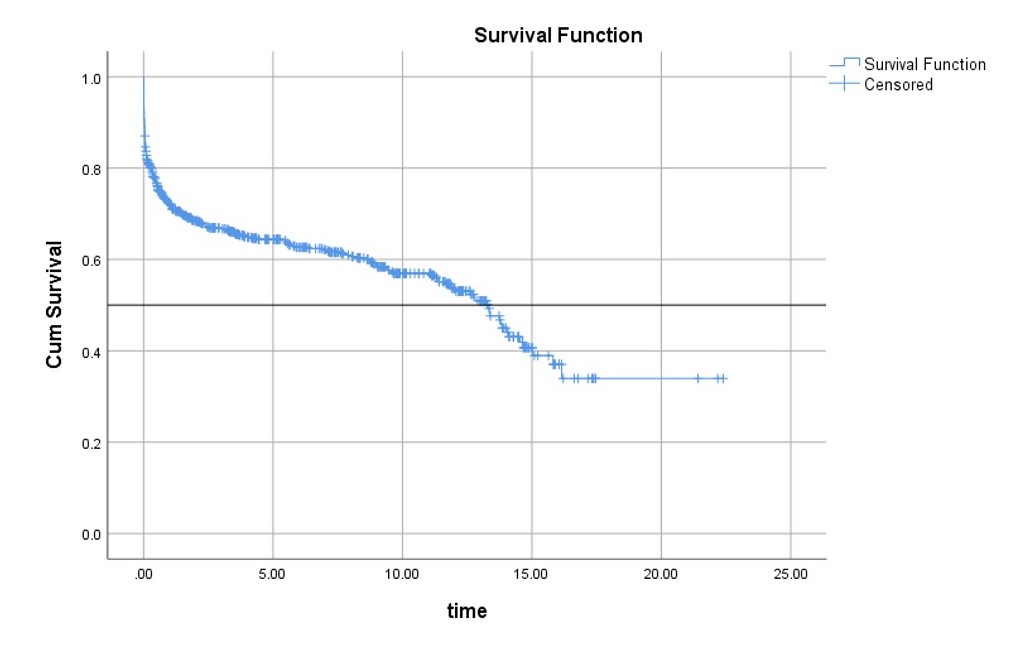
In the pediatric group, biliary atresia (25.4%), progressive familial intrahepatic cholestasis (16.6%), and Wilson’s disease (12.1%) were the most frequent etiologies for LDLT and the mean MELD/PELD score was 20. Univariable analysis indicated significant differences between patients who survived and those who did not in terms of age, graft weight, portal vein thrombosis, ascites, and donor sex. Out of the pediatric recipients, 272 (41.1%) died during the median follow-up period of 3.26 years.
Conclusion: Despite the controversies surrounding LDLT, it remains a viable treatment option for both adult and pediatric patients with ESLD. Careful consideration of donor and recipient factors, as well as close monitoring of postoperative complications, are crucial for improving outcomes. Continued research and evaluation of LDLT practices and ethical implications are essential for advancing the field.
[1] Living Donor Liver Transpant
