Impact of donor hepatic duct bifurcation location and angle on post-transplant biliary complications in recipients following living donor liver transplantation
Sunghae Park1, Namkee Oh1, Sunghyo An1, Sung Jun Jo1, Jinsoo Rhu1, Jong Man Kim1, Jae-Won Joh2, Gyu-Seong Choi1.
1Surgery, Samsung Medical Center, Seoul, Korea; 2Surgery, Samsung Changwon Hospital, Changwon-Si, Korea
Introduction: Biliary complication remains an unresolved issue in liver transplantation, despite improvements in surgical techniques and perioperative care. The aim of this study was to evaluate the influence of the location of hepatic duct bifurcation in donors with Type I bile duct on post-transplant biliary complications in recipients.
Materials and Methods: We retrospectively analyzed 109 cases of living donor liver transplantation from January 2021 to December 2022. All donors had Type I bile duct, and donor hepatectomies were performed laparoscopically by a single surgeon. We used indocyanine green fluorescence to determine the location of the hepatic duct bifurcation, which was classified into intrahepatic and extrahepatic. The bifurcation angle was assessed via 3D modeling and reconstruction from preoperative MRCP images.
Results: There were 76 and 33 cases in the extrahepatic and intrahepatic bifurcation groups, respectively. The groups significantly differed in terms of MELD score, post-transplant hepatic artery-related complications, and hepatic duct bifurcation angle. The surgical outcomes of donors were not different between the two groups. The intrahepatic bifurcation group showed lower biliary complication-free survival in recipients (p=0.018).
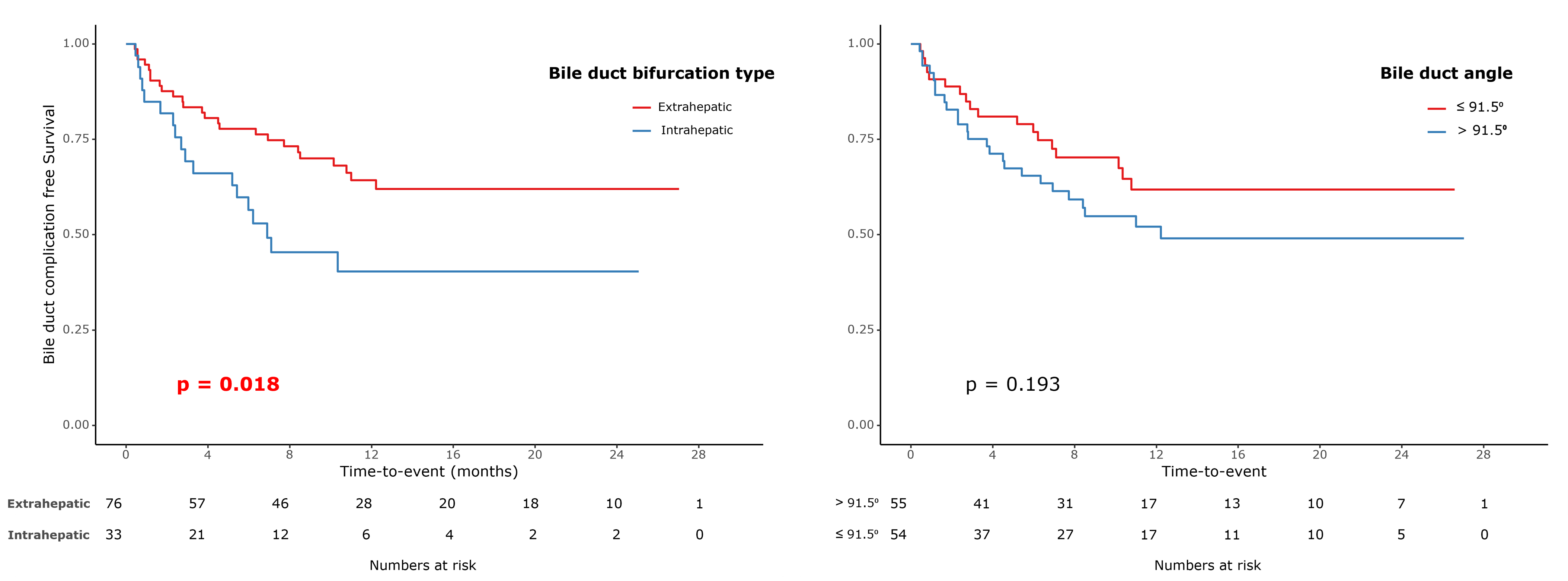
We identified a cut-off point of 91.5 degrees (AUC=0.887) for the bifurcation angle to predict extrahepatic and intrahepatic bifurcation. Comparing biliary complication-free survival based on this cut-off, we observed a trend towards worse survival in those with an angle greater than 91.5 degrees, although the difference was not statistically significant. Upon multivariable analysis, the recipients BMI (HR=1.12, p=0.006) and an intrahepatic location of the donors bile duct bifurcation (HR=1.941, p=0.035) emerged as independent risk factors for biliary complications in recipients.
Conclusion: The findings of this study highlight that the location of hepatic duct bifurcation in donors significantly impacts post-transplant biliary complications in recipients. The results also suggest the potential predictive value of the bifurcation angle, emphasizing the importance of precise anatomical assessment before transplantation.
[1] Liver Transplantation
[2] Biliary complication
[3] Living donor
