Bleeding and thrombosis in intestinal and multivisceral transplantation - Experience from 145 consecutive cases
Francesca Reeder1, Jessica C Griffin1, Matthew Carter1, Holly Lowing1, Andrew Quarrell2, Praharsh Babu2, Tracy Moore1, Andrew Butler3, Lisa Sharkey3, Charlotte Rutter4, Irum Amin3, Rohit Gaurav3, Dunecan Massey3, Neil Russell3, Jeremy Woodward3, Will Thomas1.
1Department of Haematology, Cambridge University Hospitals NHS Foundation Trust, Cambridge , United Kingdom; 2School of Clinical Medicine, University of Cambridge, Cambridge , United Kingdom; 3Department of Surgery, Cambridge University Hospitals NHS Foundation Trust, Cambridge , United Kingdom; 4Department of Gastroenterology, Cambridge University Hospitals NHS Foundation Trust, Cambridge , United Kingdom
Background: Solid organ transplantation, and its associated complication rates, are well established internationally. Associated rates of bleeding and thrombotic complications are as yet unestablished in intestinal and multivisceral transplantation.
Aims: To describe the bleeding and thrombotic incidence and experience in intestinal/multivisceral transplants performed over a 15 year period since establishment of the United Kingdom’s designated adult multivisceral transplant centre.
Methods: Retrospective analysis of 145 consecutive cases. Bleeding or thrombotic events occuring in the 92 days postoperative were observed. Data collection for either event stopped at first occurrence. Bleeding was defined using the ISTH definition of major bleeding in surgical patients.
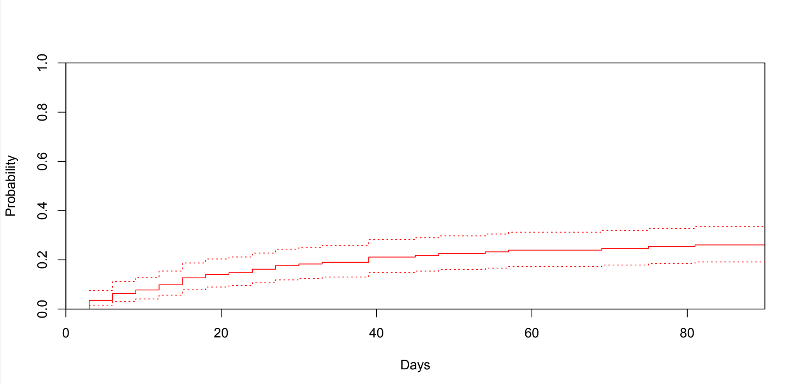
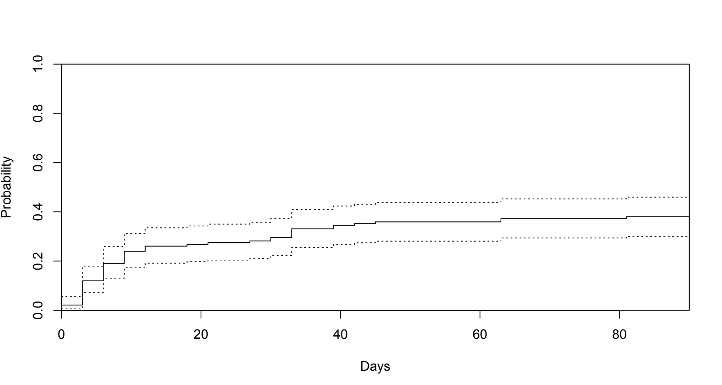
Results: Between 2008 and 2023, 139 patients received 145 transplants; 48% females, mean age 44 years and 70% with a prior history of thrombosis. Of the 145 transplants, 6/145 (4.1%) had a thrombotic event either in surgery or in the 24 hours after surgery. The cumulative incidence of thrombosis was 26.1% (95% CI 19.1 – 33.5%) from day 2-92 (Figure 1). Median transfusion requirements (units) for day of surgery and 24 hours after were 10 (red cells), 4 (plasma), 1 (platelets) and 2 (cryoprecipitate). The cumulative incidence of major bleeding was 38.0% (95% CI 30.0 – 36.0%) from day 2-92 (Figure 2). Thrombotic events occurred in 22 (15%), bleeding events in 38 (27%), and both bleeding and thrombotic events in 15 (11%). There were no bleeding or thrombotic events in 67 (47%) transplants. 8 patients were transplanted for abdominal vascular catastrophe, where long-term survival would not be possible without transplantation (further details will be presented). 6 patients received direct oral anticoagulants post-transplant; drug levels were in the expected range.
Conclusion: There is a high incidence of major bleeding and thrombosis following intestinal/multivisceral transplantation, illustrating the brittle haemostasis in these patients.
[1] Bleeding
[2] Thrombosis
[3] Multivisceral transplant
[4] Intestine containing transplant
