Rodrigo Papa-Gobbi, Argentina has been granted the TTS 2022 Research Grant Award
Sirolimus treatment increases graft survival in pediatric intestinal transplant patients and is associated with a more naïve/less activated immune phenotype, and a higher frequency of regulatry T-cells
Rodrigo Papa-Gobbi1,2, Ane Andrés-Moreno2,3, Elena Sánchez-Zapardiel4, Alida Alcolea-Sánchez2,5, Rocío González-Sacristán5, Eva Peña Saínz-Pardo5, Javier Serradilla-Rodríguez2,3, Alba Sánchez-Galán2,3, Esther Ramos Boluda2,5, Fransico Hernández-Oliveros2,3.
1Transplant Group, Institute for Immunological and Physiopathological Studies, La Plata, Argentina; 2Congenital Malformations and Transplantation Group, Institute of Biomedical Research-La Paz University Hospital, Madrid, Spain; 3 Pediatric Surgery Department, La Paz University Hospital, Madrid, Spain; 4Immunology Department, La Paz University Hospital, Madrid, Spain; 5 Pediatric Gastroenterology Departament, La Paz University Hospital, Madrid, Spain
Introduction: Regulatory T-cells (Treg) are key players in tolerance induction and maintenance, and their frequency have been associated with enhanced graft survival. Nonetheless, their implication in the alloresponse after intestinal transplantation (ITx), where the incidence of rejection is higher than that the rest of solid organs transplants, remains unclear. Our main objective was to study the Treg frequency in patients under Sirolimus (Siro) or tacrolimus (Tac) treatment and its association with graft survival.
Methods: All patients were under 18 years old and were transplanted at La Paz University Hospital (Madrid-Spain). The survival of liver containing grafts (small bowel + liver and multivisceral) was assessed in 35 patients under Siro monotherapy and 34 patients under Tac monotherapy. Patients with graft loss before two-month post-ITx were excluded from this study. Frequency of blood Treg (CD4+CD25highCD127-), activated T-cells (CD3+HLA-DR+), naïve T-cells (CD27+CD45RO-), and effector memory T-cells (CD27-CD45RO+) was assessed by flow cytometry (Patients without rejection: Siro, n=20; Tac, n=16. Patients with active rejection, n=5).
Results: Graft survival was higher in patients receiving Siro than that Tac patients (p<0.01). Principal components analysis showed that patients without rejection and under rapamycin monotherapy form a distinct cluster from those under tacrolimus treatment. Particularly, a lower frequency of CD3+HLA-DR+ (activated T-cells, p<0.05), and CD27-CD45RO+ (effector memory cells, p<0.05) T-cells, but higher percentage of CD27+CD45RO- (naïve T-cells, p<0.01) was observed in Siro treated patients. Of note, a significantly higher Treg count was observed in in the blood of Siro treated patients compared to Tac (p<.0001). Blood samples from patients undergoing acute cellular rejection (ACR) exhibited a significant reduction in the Treg number compared to patients with normo-functional grafts (p<0.05).
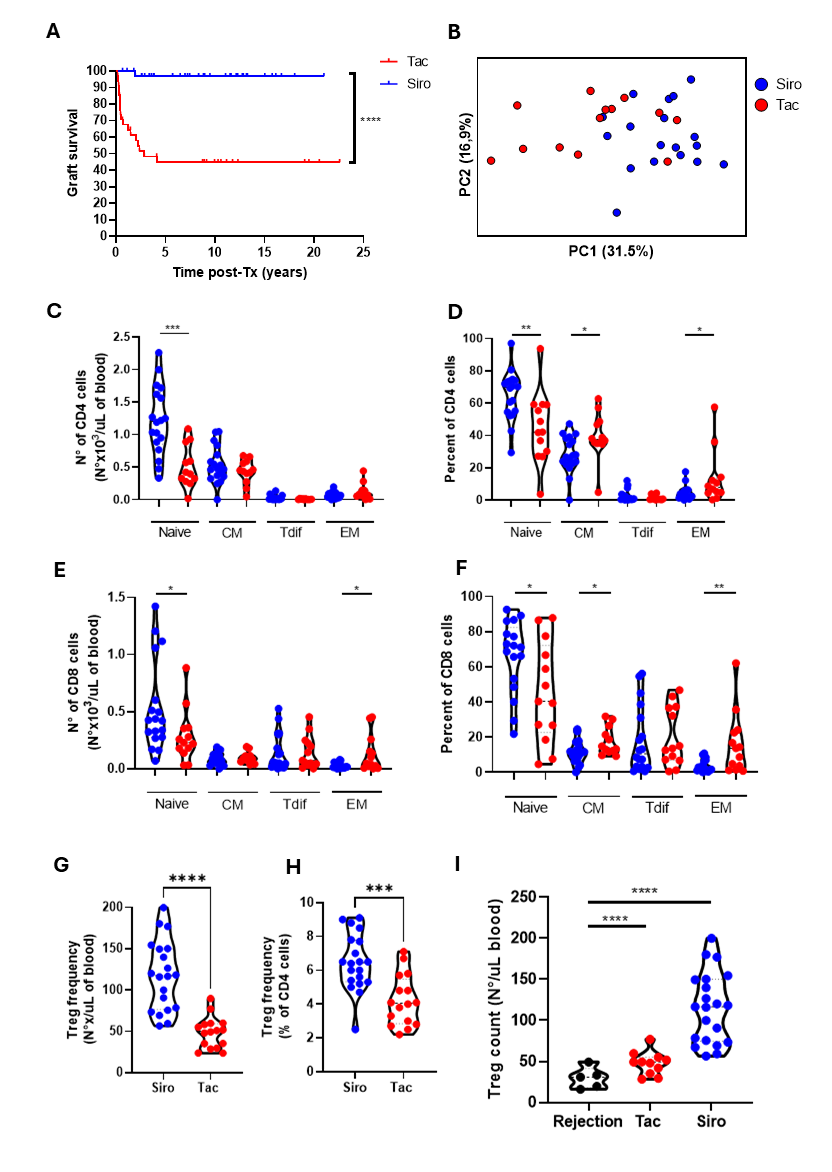
Conclusions: Our findings revealed a compelling association between reduced Tregs and the development of ACR. However, Siro monotherapy promotes Treg expansion and induces a more naïve/less activated T-cell profile. These findings suggest a potential mechanism underlying the higher graft survival rate observed in Siro vs Tac patients. Therefore, transitioning from Tac to Siro could foster Treg expansion and enhance graft survival.
