Ahad Eshraghian, Iran has been granted the TTS Scientific Congress Award
The impact of loco-regional therapy on long term outcomes of liver transplant recipients for hepatocellular carcinoma
Ahad Eshraghian1, Alireza Taghavi1, Saman Nikeghbalian1, Hamed Nikoupour1, Alireza shamsaeefar1, Seyed Ali Malek-Hosseini1.
1Avicenna Hospital, Shiraz, Iran
Introduction: Liver transplantation is the first line treatment for hepatocellular carcinoma (HCC) in the setting of liver cirrhosis. This study aimed to investigate the impact of loco-regional therapy (LRT) including trans-arterial chemoembolization and radiofrequency ablation during waiting time on post-transplant outcomes of patients with HCC.
Methods: Liver transplant recipients who had undergone liver transplantation for HCC between 2010 and 2019 were included in the study. Patients’ characteristics including LRT before transplant were recorded. Kaplan-Meier estimation was used for survival analysis with log-rank test and Cox regression analysis was used to assess independent factors for overall survival.
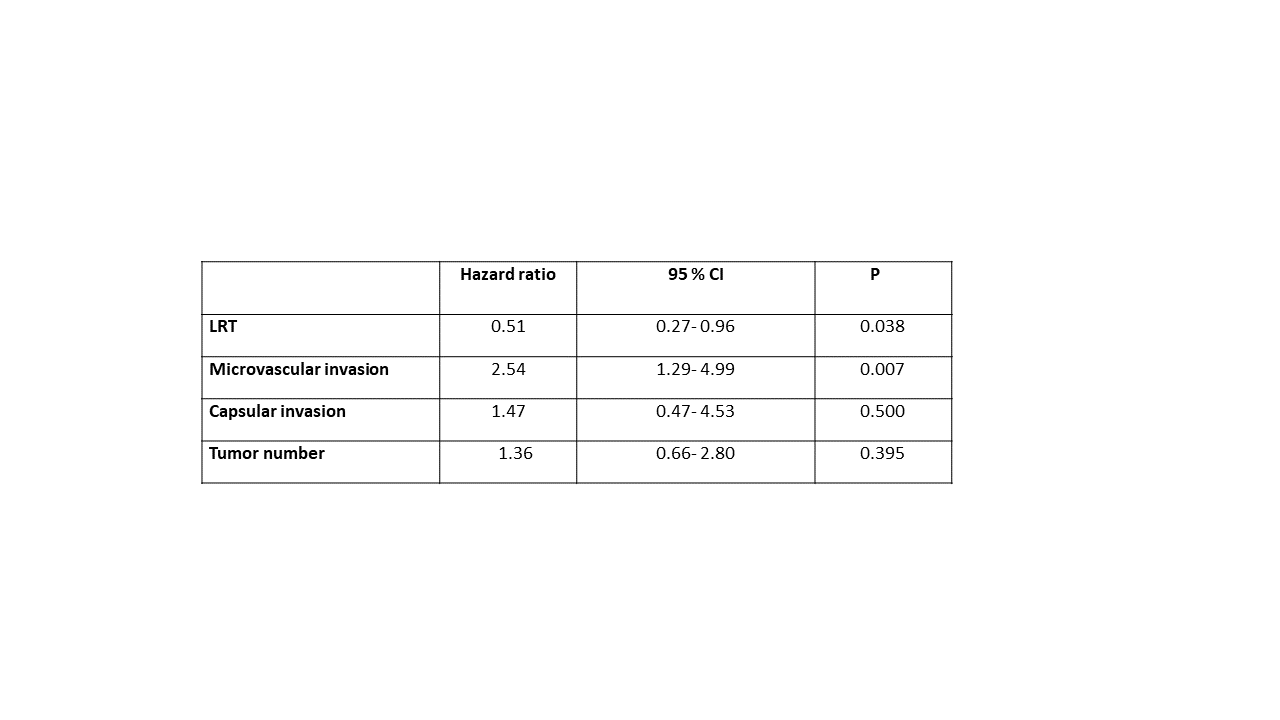
Results: Totally, 139 liver transplant recipients with mean age of 50.59 ± 13.46 were included. Eighty seven patients were within Milan criteria. Seventy eight patients (56.1 %) received LRT before liver transplantation. One year survival was 84.6 ± 4.1 % in patients who received LRT compared to 80.3 ± 5.1 % in those who did not receive LRT. In univariate analysis, LRT was associated with lower mortality after liver transplant (HR: 0.52; 95 % CI: 0.296- 0.944; P= 0.031) while microvascular tumor invasion (HR: 2.87; 95 % CI: 1.543- 5.359; P= 0.001) and tumor capsular invasion (HR: 3.06; 95 % CI: 1.291- 7.285; P= 0.011) were associated with increased mortality after liver transplantation. In multivariable COX regression analysis, LRT (HR: 0.51; 95 % CI: 0.276- 0.963; P= 0.038) and microvascular tumor invasion (HR: 2.54; 95 % CI: 1.298- 4.997; P= 0.007) were associated with lower and higher mortality after liver transplantation, respectively (Table). In a subgroup of patients within Milan criteria, LRT was an independent factor for decreased mortality after liver transplantation (HR: 0.43; 95 % CI: 0.188- 0.986; P= 0.046).
Conclusion: LRT and micro vascular invasion were independent factors associated with survival of liver transplant recipients.
[1] Liver transplantation
[2] hepatocellular carcinoma
[3] trans-arterial chemoembolization
[4] loco-regional therapy
