The outcomes of simultaneous liver–kidney transplantations with a positive crossmatch during safety net policy era in the United States
Kenji Okumura1, Ryosuke Misawa1, Abhay Dhand1, Hiroshi Sogawa1, Gregory Veillette1, Seigo Nishida1.
1Surgery, Westchester Medical Center / New York Medical College, Valhalla, NY, United States
Background: Under the safety-net policy, liver transplant candidates with kidney dysfunction, when offered organs from donor with a positive crossmatch (+XM), now have the option of either simultaneous liver-kidney transplantation (SLKT) or Kidney after liver transplant. The aim of this study was to assess the effect of +XM on outcomes of SLKT during the safety net policy era.
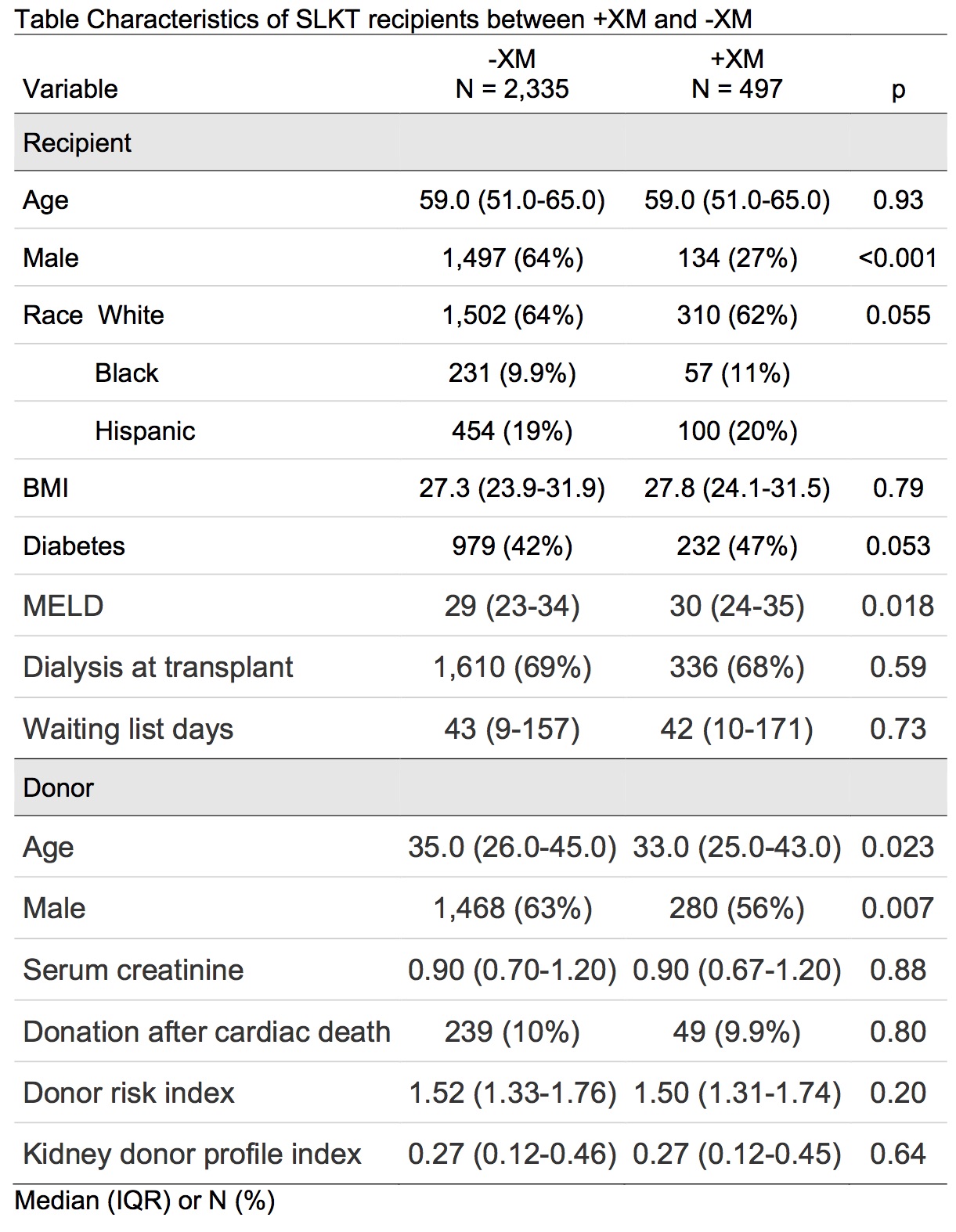
Methods: Using the United Network for Organ Sharing database 2,832 adult SLKT recipients between August 2017 to September 2023, were divided into in two groups, +XM (N=497) and negative crossmatch (–XM) (N=2335). Post-transplant outcomes in these cohorts were analyzed using Kaplan-Meier and Cox proportional hazard models. As a subgroup analysis, liver transplant alone and SLKT were also analyzed in +XM and –XM groups.
Results: Compared with -XM, SLKT recipients with +XM had a lower percentage of males (27% vs 64%, P<0.001), fewer alcohol-related liver disease (29% vs 40%), more metabolic dysfunction-associated steatohepatitis (40% vs 29%), and a higher median model for end-stage liver disease (MELD) score (30 vs 29, P=0.018).
In +XM group, cold ischemia time was shorter for both donor liver (5.6 hours vs 6.0 hours, P=0.020) and donor kidney (12 hours vs 12 hours, P=0.18). Depletional induction was used more in the +XM group (21% vs 12%, P<0.001). Post-transplant length of hospital stay was longer in the +XM group (15 days vs 13 days, P=0.016). The rate of delayed kidney-graft function was the same between the two groups (27% vs 28%, P=0.85). Serum creatinine was lower in +XM group at discharge (1.13 mg/dl vs 1.30mg/dl, P<0.001), at 6 months (1.12 mg/dl vs 1.23 mg/dl, P<0.001), and at one year (1.19 mg/dl vs 1.25 mg/dl, P<0.001). During post-transplant period, one-year patient survival, liver and kidney graft survival were comparable between +XM and –XM.

Among +XM, one-year patient survival and liver survival were better in SLKT than those in liver transplant alone. +XM was not associated with kidney graft survival (hazard ratio 1.07; 95% Confidence Interval 0.82-1.39, P=0.63), and in +XM cohort, liver transplant alone was associated with mortality and graft failure compared to SLKT (hazard ratio 2.88; 95% Confidence Interval 1.19-6.92, P=0.018).
Conclusions: Crossmatch positivity in a selected group of SLKT recipients was not associated with worse patient or graft outcomes and may not influence the decision to use these organs.
The data reported here have been supplied by the UNOS as the contractor for the OPTN. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the OPTN or the U.S. Government.
[1] UNOS
[2] Liver transplant
[3] Kidney Transplant
[4] Cross match
[5] Simultaneous liver-kidney transplantation
