Successful implementation of pure laparoscopic right donor hepatectomy in a small center with limited experience: The role of proctorship program
Manuel Lim1, Gyu-Seong Choi2, Jieun Kwon3.
1Department of Surgery, Myongji Hospital, Goyang, Korea; 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 3Department of Surgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
Introduction: Pure laparoscopic donor right hepatectomy (PLDRH) has recently been widely performed. However, most of the PLDRH cases are carried out in larger volume centers with extensive experience in laparoscopic liver surgery and transplantation. In this study, we report the process and outcomes of eight cases performed in a small center with limited experience, under the guidance of a proctorship program.
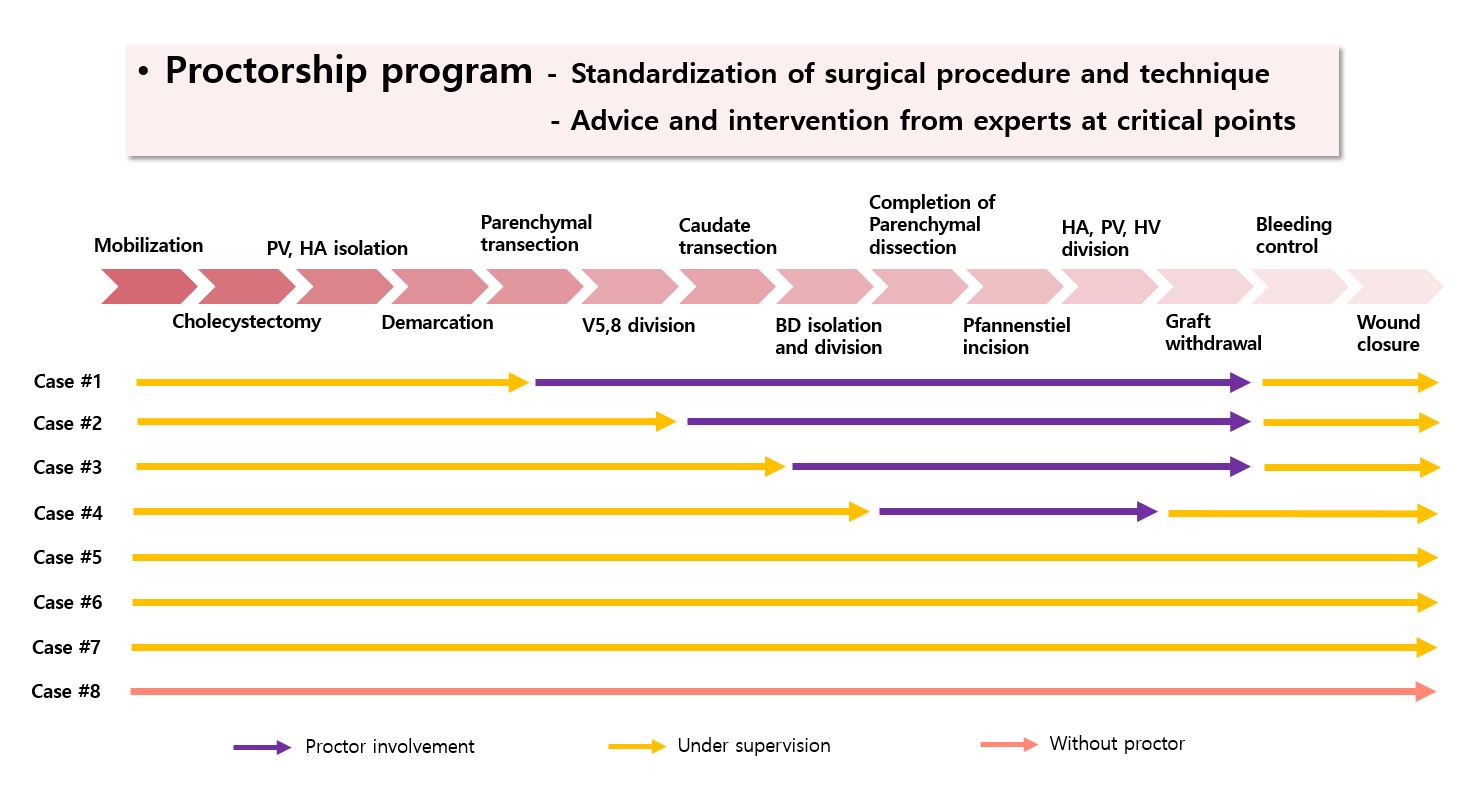
Method: Between August 2022 and October 2023, eight cases of PLDRH were performed for adult-to-adult living donor liver transplantation (LDLT). All operations were performed under the proctorship program and followed Samsung Medical Center’s protocol. The operator was a junior surgeon with some experience in laparoscopic liver resection but had no experience with open donor hepatectomy. In the first four cases, the proctor intervened only at critical points of the surgery, gradually reducing his involvement. In the last four cases, the operator performed the surgery independently.
Results: In all eight cases, modified right grafts were obtained using pure laparoscopic hepatectomy. Six of eight cases included anatomic variations in the bile duct and portal vein. The median operative time was 358 (255 – 480) minutes, and there were no instances of open conversion. The median estimated blood loss was 500 (200 - 800) milliliters, and there were no perioperative or postoperative transfusions. All donors were discharged on day 7 postoperatively, and no postoperative complications were observed at all.
Conclusion: In our experience, PLRDH can be safely performed even in small centers with limited experience under the proctorship program, overcoming the learning curve.
[1] Minimal invasive donor surgery
[2] Living donor liver transplantation
[3] Proctorship
[4] Pure laparoscopic donor hepatectomy
