
Normothermic machine perfusion of explanted livers: Pilot of a novel translational model for end-stage liver disease
Rachel Todd1, Leonie van Leeuwen1, Matthew Holzner1, Leona Kim-Schluger1, Daniel Puleston2, Sander Florman1, M. Zeeshan Akhtar1.
1Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Precision Immunology Institute and the Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Normothermic machine perfusion (NMP) is an emerging preservation technique in transplantation for assessing organ function and increasing the pool of donor organs. Currently, NMP has mainly been utilized clinically in the field of organ transplantation. However, there is considerable potential to expand upon the utilization of this technique. Here, we introduce a novel use of the platform as a translational research model of end-stage liver disease using hepatectomized livers from liver transplant recipients. We also include discarded donor livers that underwent NMP as a comparator group.
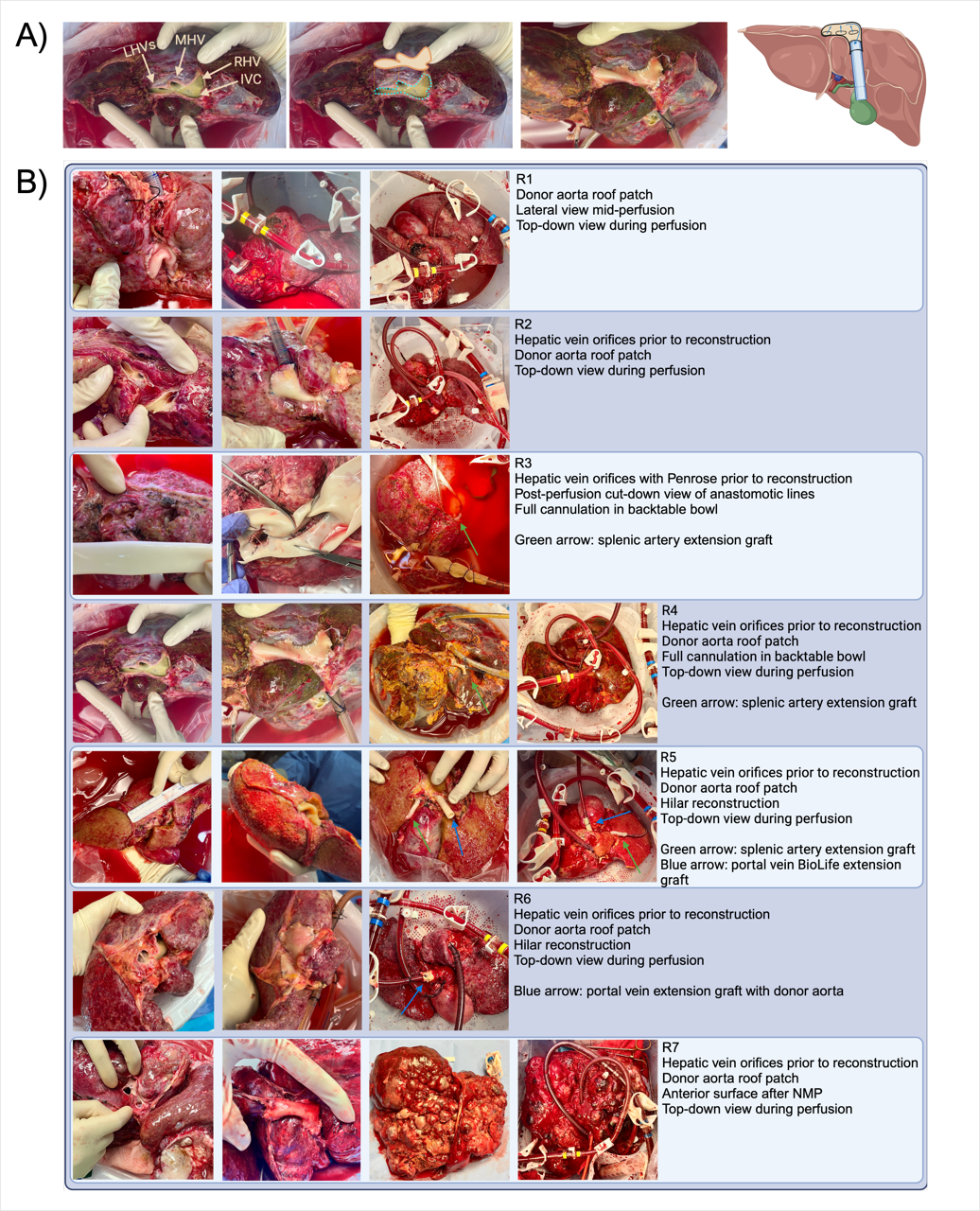
After the explantation of the native liver during orthotopic liver transplantation, seven hepatectomized livers were flushed on the back table using 1 liter of HTK solution, followed by 3 liters of heparinized saline. Vascular reconstruction of the venous outflow, arterial anatomy, and portal vein were undertaken to allow for cannulation of these three systems (Fig 1). After cannulation, the livers were perfused normothermically using the OrganOx metra. Flow parameters and perfusate samples were collected and assessed via arterial blood gas analysis for viability markers. The 8 discarded donor livers were flushed with 4-6 L of HTK and cannulated in a similar fashion, though in lieu of vascular reconstruction of the venous outflow, the cuff of suprahepatic IVC was sutured closed to allow proper cannulation.
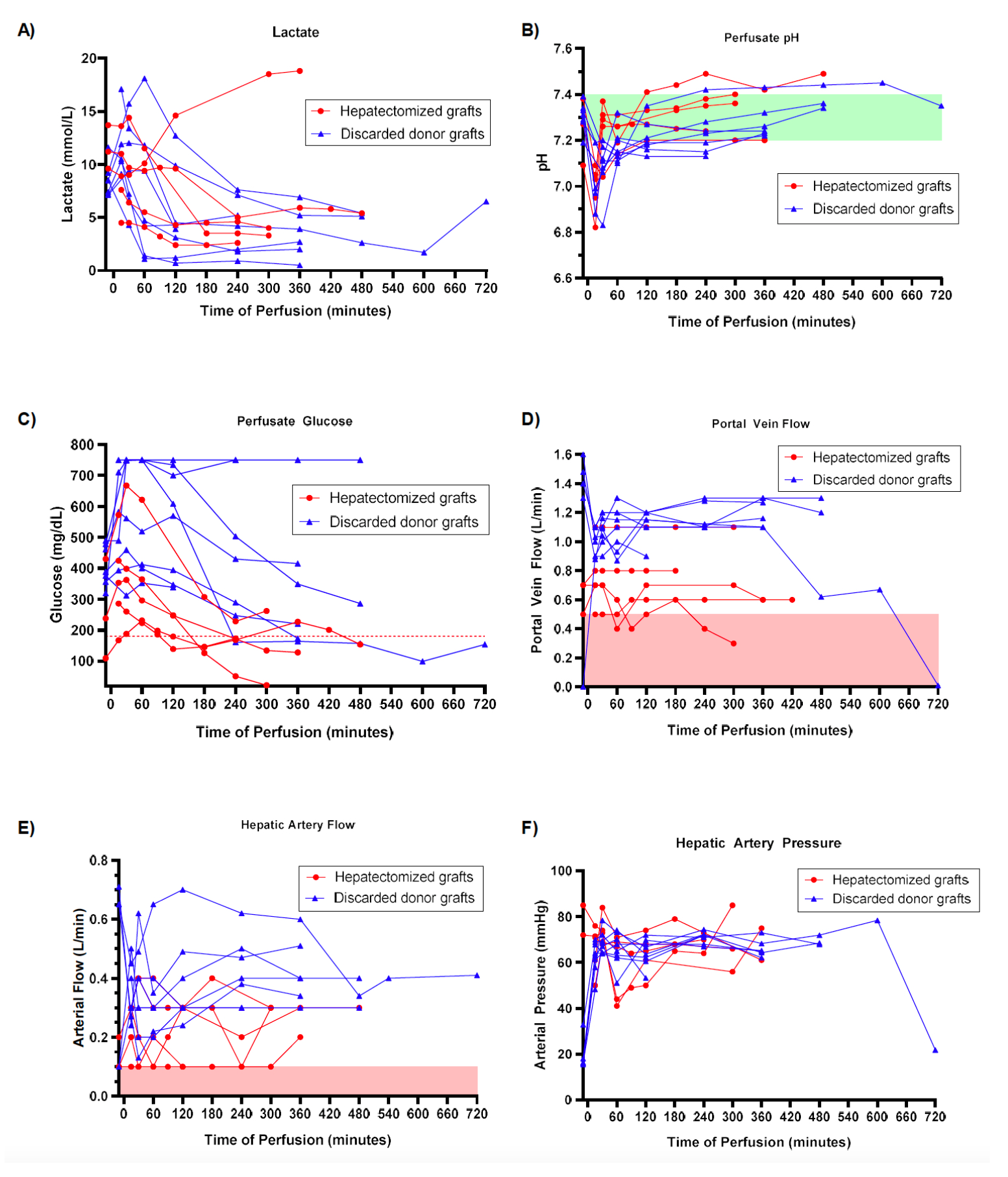
Of the seven hepatectomized livers in our study, five achieved technical success, defined as perfusion for at least one hour, with an average perfusion time of 5.85 hours. Average reconstruction time, or cold ischemia time (CIT) prior to perfusion, was 198 minutes, or 3.27 hours. Four of the five diseased livers cleared lactate, and all utilized glucose (Fig 2). pH stability and sodium bicarbonate requirements varied, though all maintained pH levels above 7.3 after 2h of NMP without bicarbonate resuscitation. Similar portal vein flows were achieved for all 5 grafts, though hepatic artery flows varied. For the 8 discarded donor livers, average CIT was 5.64 hours, and average perfusion time was 8.69 hours. These 8 performed similarly in lactate clearance and pH stability, but portal and arterial flows were significantly higher than in diseased organs (Fig 2).
To our knowledge, we provide the first description of how to perform this complex procedure of reconstruction and ex vivo perfusion of a hepatectomized liver. The ability of these organs to demonstrate some intact functionality and to perform during NMP similarly to discarded livers despite the injury sustained during explantation is substantial. It suggests the feasibility of using normothermic machine perfusion to explore advanced liver disease in an entire functioning, isolated organ, a setting optimal for exploring a vast array of questions ranging from drug pharmacology and efficacy to cancer metabolism and immune profiling.
[1] normothermic machine perfusion
[2] Liver pathophysiology
[3] organ preservation
[4] Hepatectomy
