Circulating neutrophil extracellular traps (NETs) in deceased donors prior to retrieval and during normothermic perfusion – An opportunity for donor liver optimisation in-situ, ex-situ and beyond
Syed Hussain Abbas1, Funga Dengu1, Hatem Sadik1, Carlo Ceresa2, Andrew Aswani3, Peter Friend1.
1Nuffield Department of Surgical Sciences, University of Oxford, Oxford, United Kingdom; 2Liver Transplant Unit, Royal Free Hospital, Oxford, United Kingdom; 3Santersus, AG, Zurich, United Kingdom
Introduction: Neutrophil extracellular traps (NETs) are associated with poor liver transplant outcomes including ischemia-reperfusion injury (IRI), acute rejection and thrombosis. The presence of pre-retrieval circulating NETs has not previously been investigated in extended criteria deceased (ECD) donors. This study aims to investigate the presence of circulating NETs prior to ECD organ retrieval and during 48-hour normothermic perfusions of discarded human livers.
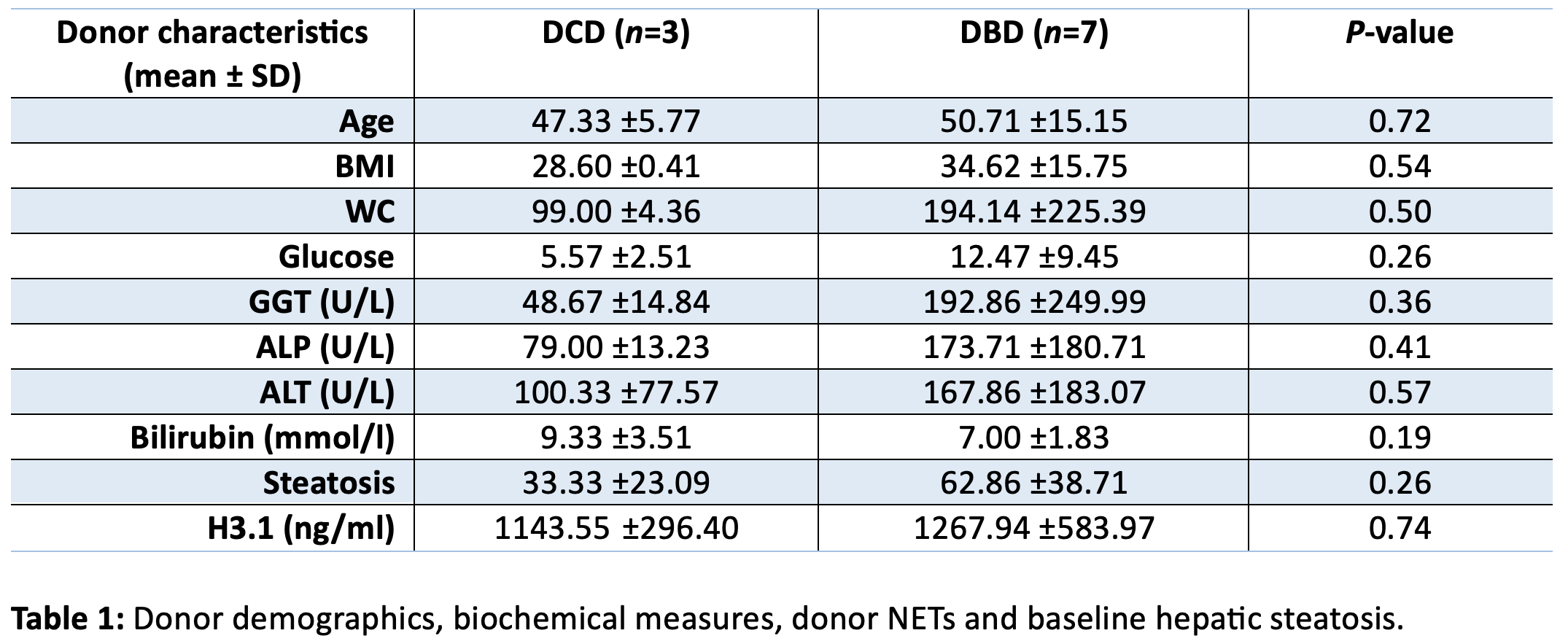
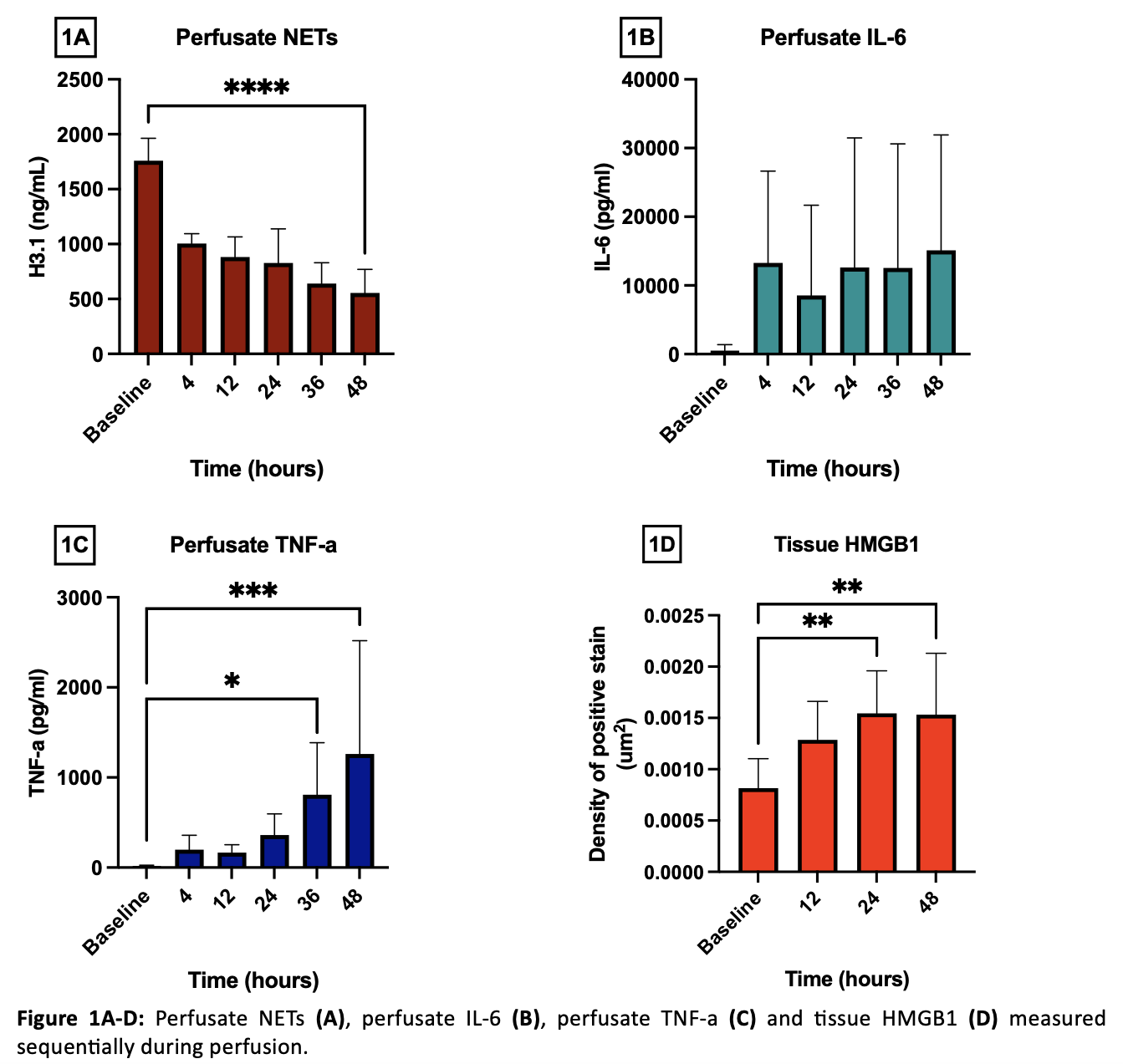
Methods: A total of 10 ECDs were included in this study (DCD, n=3 and DBD, n=7). Donor demographics, biochemical measures and circulating NETs were compared between groups prior to retrieval. NETs were measured using the H3.1 Elisa Kit (Volition, Belgium). The presence of circulating perfusate NETs, cytokines (MERCK Milliplex Human Cytokine Panel) and tissue HMGB1 (immunohistochemistry) was also investigated in 6 discarded human livers preserved over 48 hours using the OrganOx metra with perfusate (0.5-1h) and biopsy (pre-NMP) samples taken at baseline and sequentially during preservation. Statistical analysis was performed using unpaired T-tests and one-way ANOVA with data reported as mean ± SD.
Results: Donation after circulatory death and DBD donors had similar baseline characteristics with high levels of circulating NETs prior to retrieval (DCD: 1143.55ng/ml ±296.40 vs. DBD: 1267.94ng/ml ±583.97, P = 0.74), (Table 1). Discarded human livers preserved over 48 hours demonstrated high circulating NETs at baseline (1759ng/ml ±205.20) and a significant reduction at the end of 48h perfusion (554.70 ng/ml ±215.20), P<0.0001 (Figure1A). There was also an increase in perfusate IL-6 (Figure1B) and a significant increase in perfusate TNF-a (Figure 1C) and tissue HMGB1 (Figure 1D) during perfusion.
Discussion: This study provides mechanistic insights into donor and preservation related injury/inflammation. Removal of NETs using during retrieval (DBD and during dcd-NRP), ex-situ perfusion and recipient reperfusion may mitigate complications associated with transplantation of ECD livers through application of novel extra-corporeal columns i.e. NucleoCapture which we have recently explored.
[1] DCD
[2] DBD
[3] Neutrophil extracellular traps
[4] NMP
