Sphingosine-1-phosphate receptor 1 regulates endothelial permeability during ischaemia reperfusion injury
Jenny Gilmour1, Georgina C Wilkins1, Nick Chilvers1, Neil Sheerin1, Andy Fisher1, Simi Ali1.
1Translational and Clinical Research Institute, Newcastle University, Newcastle Upon Tyne, United Kingdom
Introduction: Ischaemia reperfusion injury (IRI) after organ transplantation can result in primary graft dysfunction (PGD). Severe PGD is associated with a significant increased risk of early mortality and late complications of rejection. There are currently no condition-specific therapeutics available to prevent or treat the condition. Sphingosine-1-phosphate (S1P) reduces vascular endothelial permeability via activation of S1P-receptor 1 (S1PR1). We hypothesised that agonism of S1PR1 would protect and/or improve vascular endothelial integrity, therefore limiting IRI in the organs declined for clinical transplantation.
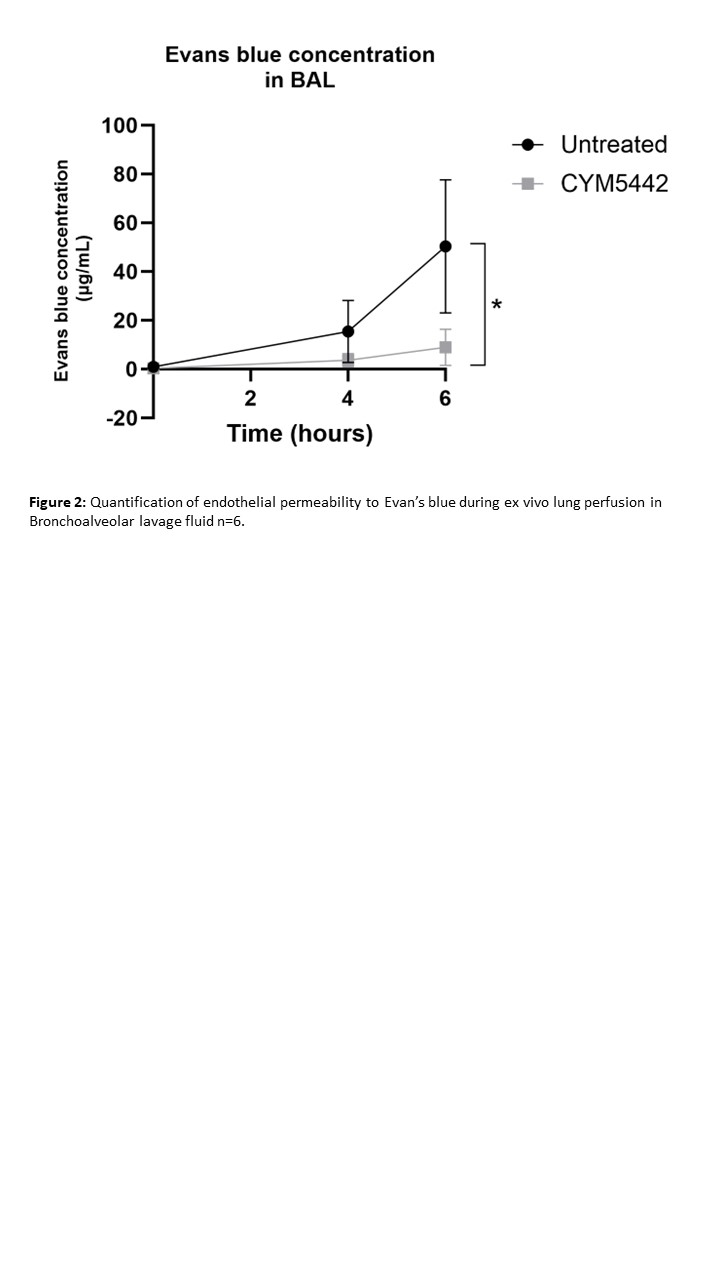
Methods: An optimal dose of the S1PR1 agonist, CYM5442, was established in human microvascular endothelial cells in-vitro permeability assays. For renal IRI experiments, male C57BL/6 mice were treated with 3 mg/kg CYM5442 1hour prior to surgery. The kidneys of these mice were clamped for 30 min, and the mice were left to recover for 23 h. The mice were then injected with 3 mg/kg CYM5442, then with 20 mg/kg EB dye 1 h later. In ex vivo lung perfusion (EVLP), CYM5442 was administered to declined human donor lungs in a paired split-lung model. CYM5442 and vehicle treated lungs were exposed to 6 hours of EVLP. Lung weight, endothelial permeability to Evan’s blue dye, wet/dry ratio and direct lung ultrasound evaluation (CLUE) score was assessed.
Results: CYM5442 treatment of endothelial cells reduced neutrophil transmigration (p < 0.01) and endothelial permeability (p < 0.005), using in vitro permeability assays. In an in vivo mouse model of renal IRI, S1PR agonism with CYM5442 reduced endothelial permeability as shown by reduced Evan’s Blue dye extravasation (Figure 1). Western blot was used to assess phosphorylation at different sites on vascular endothelial (VE)–cadherin and showed that CYM5442 reduced VEGF-mediated phosphorylation. Concentrations of S1P in serum were significantly higher than in human organ perfusates (p≤0.05, n=7). Furthermore, during EVLP (n=6 lung pairs), both groups maintained stable perfusate flow rates and left atrial pressures. CYM5442 significantly reduced Evan’s blue accumulation in bronchoalveolar lavage (p=0.0107, Figure 2) and lung tissue (p=0.0077) compared to vehicle. Lung weights were significantly lower in the CYM5442-treated group at the end of EVLP (p=0.0136).
Conclusion: Use of CYM5442 protects vascular endothelial barrier integrity both in kidney and lungs. It limits pulmonary oedema formation during EVLP and targeting S1PR1 may be a viable treatment option for donor-organs prior to transplantation to reduce the risk of IRI.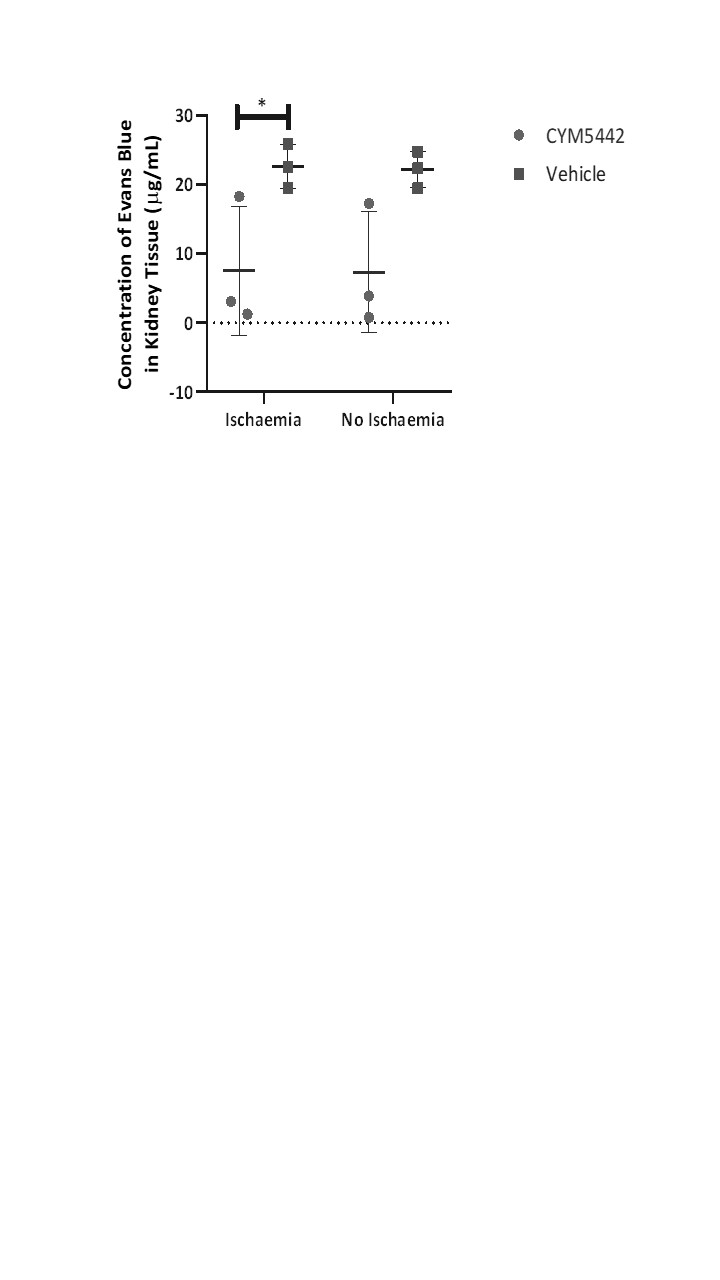
[1] ischaemia reperfusion injury
[2] endothelial permeability
[3] ex vivo lung perfusion
[4] sphingosine-1-phosphate
