Patients remaining donor specific antibody (DSA) negative post transplantation have more regulated and fewer antigen specific Th-1 cell responses to mismatched donor human leucocyte antigens (HLA) versus those who develop DSA
Sumoyee Basu1, Caroline Dudreuilh1, Hannah Burton1, Chloe Martin2, Olivia Shaw2, Kate Bramham1, Giovanna Lombardi1, Anthony Dorling1.
1School of Immunology & Microbial Sciences, Kings College London, London, United Kingdom; 2Clinical Transplantation Laboratory, Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
Introduction: Becoming sensitised to HLA negatively impacts on waiting times for future transplants and outcomes post-transplantation. However, some patients fail to develop HLA antibodies following a sensitising event. Very little is known about how these alloresponses are regulated. IFNy and IL17 associate with adverse transplant outcomes and are hypothesised to have a role in how DSA formation is controlled.
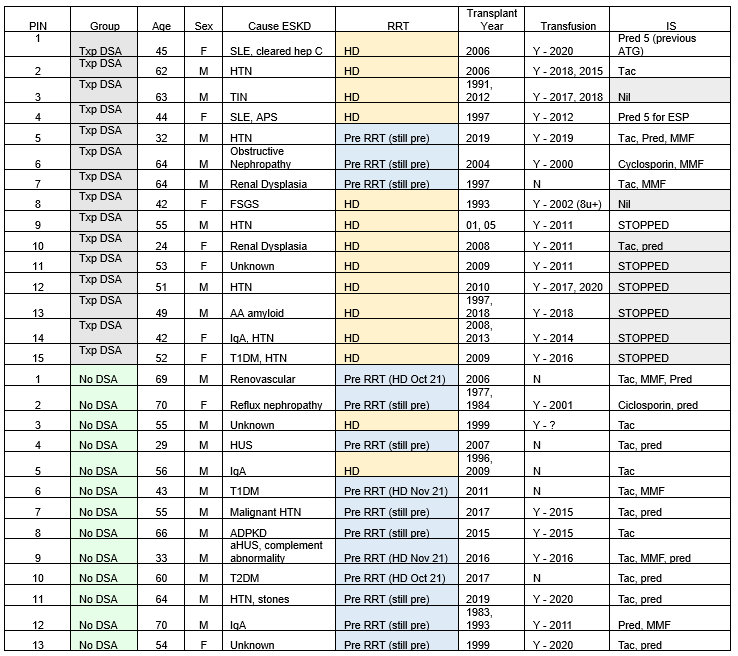
Methods: >5000 renal patients with eGFR<25mL/min/1.73m2 were screened at two London hospitals to identify patients with previous renal transplantation (without prior pregnancy). Only 13 patients (~0.3%) were persistently negative on all historic PRA tests including all possible DSA- women (n=2) identified by screening. 15 persistently positive controls with DSA MFI >2000 on all clinical tests were also recruited (Table 1).
CD8 depleted peripheral blood mononuclear cells from patients were rechallenged with HLA pure proteins (PP) corresponding to previous mismatched (MM) donor HLA and DSA to evaluate indirect alloresponses. In IFNγ and IL17 FluoroSpots, antigen specific responses (ASR) by CD4+ cells were compared in a total of 66 assays, including conditions with additional depletion of B cells and CD25high cells. Fisher’s exact 2 tailed test was used for statistical comparisons.
Results: The DSA- group had more male patients, slightly higher average age (55 vs 48), had fewer blood transfusions, were more likely to be pre-dialysis and all were on immunosuppression.
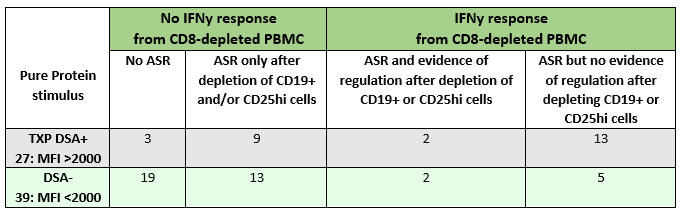
Samples from DSA+ patients were more likely to have IFNy ASR compared to samples from the DSA- group (24/27 samples ASR in DSA+ vs. 20/39 samples ASR in DSA- group: p = 0.0015). This is consistent with more patients DSA- group not becoming T cell sensitised to the MM HLA. However, this was not apparent for IL17 ASR (p = 0.3266). Comparing only samples showing ASR, fewer from the DSA+ group showed increased IFNy production after depletion of putative regulatory B or T cells, 11/24 in DSA vs 15/20 in DSA-, though this just failed to meet statistical significance (p = 0.0685). This suggests that IFNy T cell responses in the DSA- group are more likely to be regulated post-sensitisation than in the DSA+ group.
Conclusion: This is the first demonstration that patients who do not develop DSA following kidney transplantation have less T cell sensitisation and make fewer antigen specific IFNy cell responses to previous donor MM transplant antigens compared to DSA+ patients. Moreover, our data suggests that even if Th-1 cells are sensitised, failure to develop a DSA is associated with suppression of these cells by B cells or CD25hi T regulatory cells (Tregs). Ongoing analysis with a 36 colour flow cytometry panel will interrogate which regulatory and effector subsets mediate these processes. Thus potentially enabling prediction of patients that develop DSA and highlight subsets that could be boosted with Treg cell therapy.
Medical Research Council. Guy's & St.Thomas' Kidney Patients' Association.
[1] Allorecognition
[2] HLA Antibodies
[3] Sensitization
[4] Donor Specific Antibodies
