Impact of de novo or worsening of pre-existing valvular heart disease in patients referred to the kidney transplant waitlist – a single centre retrospective cohort study
Satish Vaarman Jeyabalan1, Quan Yao Ho1,2, Haoyang Chen 3, Yan Nerng Lye3, Choong Hou Koh4, Shan-Yeu Carolyn Tien1,2, Ian Tatt Liew1,2, Sobhana Thangaraju1,2, Ningyan Wong4, Yi Shern Terence Kee1,2.
1Department of Renal Medicine, General Hospital, Singapore, Singapore; 2SingHealth Duke-NUS Transplant Centre, Singhealth, Singapore, Singapore; 3Yong Loo Lin School of Medicine, National University, Singapore, Singapore; 4Department of Cardiology, National Heart Centre, Singapore, Singapore
Background and Hypothesis: Valvular heart disease (VHD) is highly prevalent amongst patients with chronic kidney disease (CKD) and is associated with poor outcomes. However, the incidence, risk factors and impact of valvular heart disease on end-stage kidney disease (ESKD) patients while on the deceased-donor kidney transplant (DDKT) waitlist is unclear.
Methods: This is a single-centre retrospective cohort analysis of ESKD patients who were referred for wait-list placement between 2009 and 2017 and underwent at least 2 transthoracic echocardiographies (TTE). Patients with previous valvular repair were excluded. De novo VHD (dnVHD) defined as new VHD of at least moderate severity that developed during the waitlist. Worsening of pre-existing VHD (wpVHD) was defined as valve disease that progressed from baseline of at least mild to another higher grade pre-transplantation. To facilitate statistical analysis, dnVHD and wpVHD are grouped together (dn+wpVHD) and compared against patients’ without dnVHD and wpVHD.
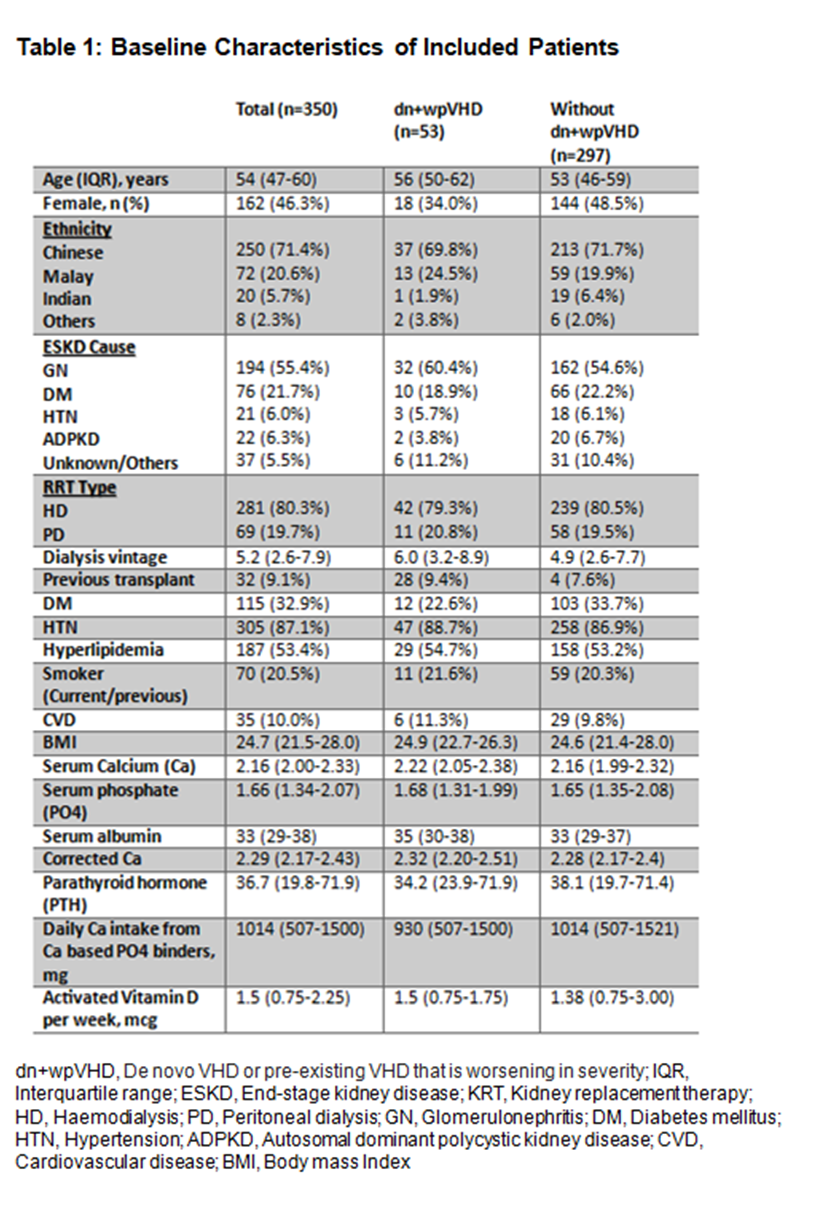
Results: Of 510 patients referred for DDKT waitlist placement, 350 with at least two serial TTE were included in the analysis (Table 1). The median interval between the baseline and the subsequent TTE is 2.4 years (interquartile range (IQR) 0.9-4.7), and they were followed up for a median of 4.4 years (IQR 1.9-6.4). Of the patients included, 53 (15.1%) developed dn+wpVHD.
The most common dn+wpVHD were tricuspid regurgitation, TR (n=29/350; 8.3%), mitral regurgitation, MR (16/350; 4.8%), aortic regurgitation, AR (9/350; 2.6%), and aortic stenosis, AS (6/350; 1.7%). When all the valvular deformities were analysed individually, only the combined de novo AS and worsening pre-existing AS (dn+wpAS) group were associated with mortality on univariable analysis (HR 11.1, 95% confidence interval (CI) 4.72-26.18, p=0.000).
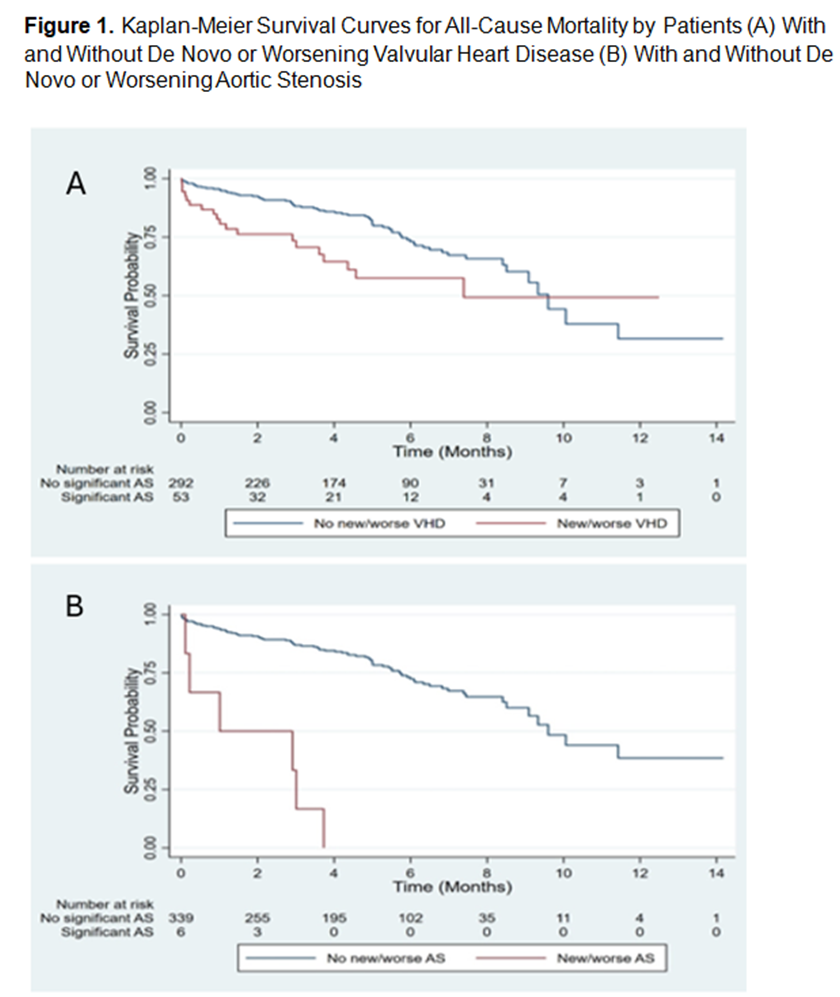
dn+wpVHD were associated with older age (HR 1.04, 95% confidence interval (CI) 1.01-1.07, p=0.009). dn+wpVHD was associated with all-cause mortality (HR 1.79 95% CI 1.07-3.00, p=0.03, Figure 1a) with decreasing hazard over time (time varying co-variate (TVC) 0.73, 95% CI 0.58-0.92, p=0.007), even after adjustment for age, cardiovascular disease, corrected serum calcium and albumin (aHR 2.02, 95% CI 1.14-3.61, p=0.02, TVC 0.70, 95% CI 0.52-0.95, p=0.02).
dn+wpAS were significantly associated with age (HR 1.23, 95% CI 1.09-1.39, p=0.001) and previous history of total parathyroidectomy and deltoid implantation, TPDI (HR 15.7, 95% CI 1.77-139.1, p=0.01). dn+wpAS were also significantly associated with all-cause mortality (HR 11.1, 95% CI 4.7-26.2, p<0.001. Fig), even after adjustment for age, cardiovascular disease, corrected serum calcium and albumin [adjusted HR (aHR) 9.04, 95% CI 3.30-24.7, p<0.001, Figure 1b].
With non-cardiovascular mortality as competing event, left-sided dn+wpVHD (sub distribution HR 4.93, 95% CI 2.05-11.9, p<0.001) are significantly associated with cardiovascular mortality and remained significantly associated on multivariable analysis (adjusted sub-HR 6.66 95% CI 1.65-26.9, p=0.008).
Conclusion: dn+wpVHD, especially dn+wpAS, are independently associated with all-cause and cardiovascular mortality amongst patients referred for DDKT. Risk factors for dn+wpAS may include age & previous history of TPDI.
[1] Aortic Stenosis
[2] Chronic Kidney Disease
[3] End Stage Kidney Disease
[4] Heart Valve Disease
[5] Aortic Valve Disease
[6] Kidney Transplantation
