
Kidney transplant from DCD donation: A novel pre-transplant combined clinico-pathological predictive score
Alessandro Del Gobbo1, Leonardo Bizzo1, Tullia De Feo2, Maria Carmela Rossi2, Umberto Gianelli3.
1Division of Pathlogy, Fondazione IRCCS Ca' Granda - Ospedale Maggiore Policlinico, Milan, Italy; 2SC Trapianti Lombardia – NITp, Fondazione IRCCS Ca' Granda - Ospedale Maggiore Policlinico, Milan, Italy; 3Department of Health Sciences and SC Anatomia Patologica, ASST Santi Paolo e Carlo and University of Milan, Milan, Italy
Introduction: Donor after cardiac death (DCD) kidney biopsies show peculiar and de novo morphological alterations strictly linked to ischemia-reperfusion injury (IRI).
The aim of this study was to combine analysis of IRI-related histopathological findings and clinical data of donors’ renal function to predict functional recovery in recipients in DCD donation.
We quantified acute tubulary inury and loss of the brush border in tubular epithelium, we correlated with donors’ renal function data, and we elaborated a clinico-pathological score.
Methods: In this study 60 biopsies from our institution have been evaluated.
Main histopathological lesions such as acute tubular injury (ATI), brush border loss (BBL) and their extension in percentage quantification have been analysed as previously described by our group and were correlated to clinical parameters and functional recovery data.
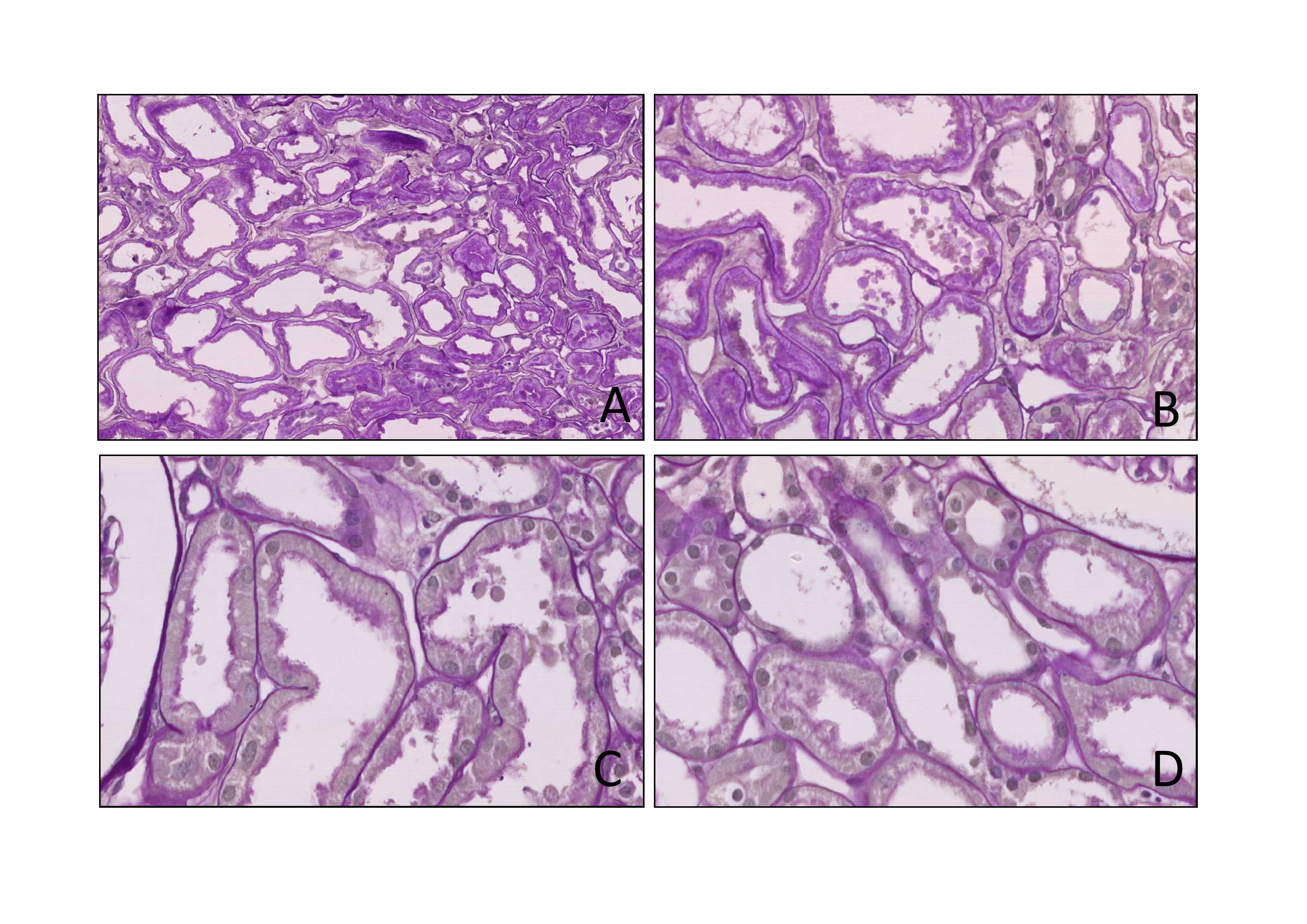
Results: Acute tubular injury was found in 30% of the observed tubules (Figure 1A and 1B, H&E, 20x and 40x), while the brush border loss in 40,9% (Figure 1D, H&E 20x. Figure 1C normal brush border, H&E 40x).
We found a linear correlation between the serum terminal creatinine and the extension of tubular lesions: the increase of creatinine levels predicted a greater extension of the IRI-related lesions (ATI: r coefficient = .4752 and p-value = 0.001 – BBL: r = .4222 and p = 0.0008).
The ROC curve obtained to evaluate the ability of the BBL extension to predict functional recovery has shown that in the presence of BBL greater than 15% there was correlation with a delayed and primary non-function (AUC = .66; .53-.78 CI 95%; p = .039).
Subsequently, a second ROC curve was obtained to identify a possible terminal serum creatinine value predictive of BBL > 15% in biopsies, demonstrating a cut-off value of 0.9 mg/dL (AUC = .81; .67-.90 95% CI; p <.001).
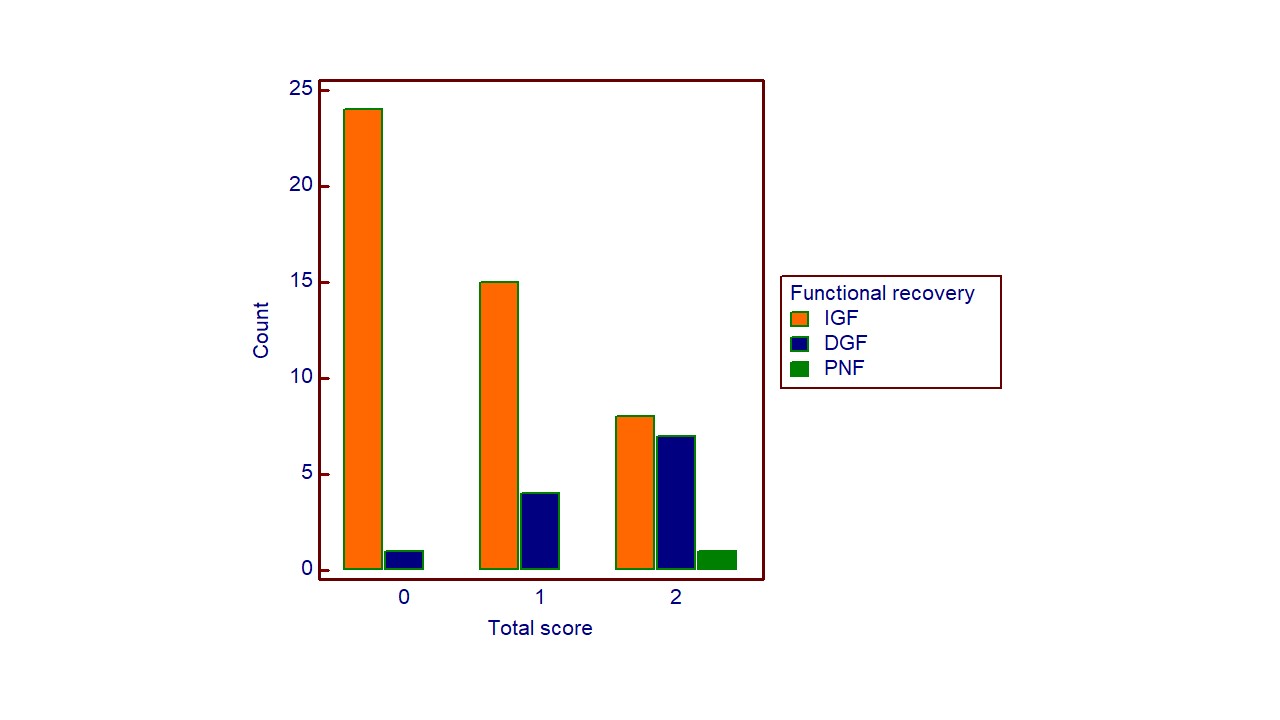
Finally, we performed a χ2 test and we built a scoring system based on these two cut-off values. Specifically, creatinine values lower than 0.9 mg/dl and extension of the BBL less than 15% were evaluated with a score of zero, while values equal or higher than the previous cut-off values were evaluated with a score of 1, returning a total score ranging between 0 and 2.
As the total score increased, there was a greater probability of delayed functional recovery and primary non function of the transplanted kidney (p = 0.001) (Figure 2).
Conclusion: DCD donor kidney transplantation represents a valid and necessary alternative to DBD donation, given the lack of donors and the high demand for transplantable organs.
DCD kidneys show peculiar IRI-associated histopatological alterations: our clinico-pathological score considers both morphology and clinical setting with an affordable cost and excellent statistical significance allowing a stratification of patients based on delayed and primary non function risk.
[1] DCD
[2] Delayed graft function
[3] Histopatology
[4] Pre-transplant biopsy
[5] Acute tubular injury
