Prognostic value of pre- and post-transplant pulmonary hypertension evaluation, estimated by right ventricular systolic pressure, on all-cause mortality in renal transplant recipients
Isabel Scalia1,2, Juan M. Farina1, Chadi Ayoub1, Sami Riad2, Hani Wadei2, Lisa Lemond1, Reza Arsanjani1, Girish K. Mour2.
1Division of Cardiovascular Diseases, Mayo Clinic, Phoenix, AZ, United States; 2Division of Internal Medicine, Nephrology, Mayo Clinic, Phoenix, AZ, United States
Introduction: Pretransplant pulmonary hypertension (PHTN) in patients with end stage renal failure carries significant morbidity and mortality, however its reversibility and impact on prognosis following renal transplant is not well established.
Methods: A multicenter retrospective review was conducted on consecutive patients who underwent solitary kidney transplantation between 1/1/2011 and 09/30/2021. Baseline comorbidities and characteristics were collected from electronic medical records. PHTN was assessed using transthoracic echocardiograph-derived right ventricular systolic pressure (RVSP). RVSP was reported both before transplant, using the most recent TTE prior to surgery, and after transplant using the first TTE after six months post-surgery. Patients with elevated RVSP (> 40mmHg) pre-transplant were evaluated as either “reversible” (RVSP improved to ≤ 40mmHg post-transplant) or “persistent” (RVSP remained elevated post-transplant).
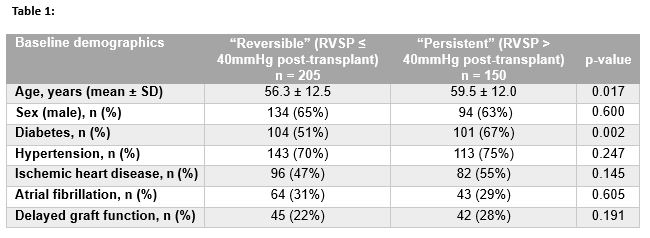
Results: A total of 939 patients who underwent kidney transplant at our centers were found to have pre-transplant RVSP > 40mmHg. Of these patients, 355 had post-transplant TTEs completed and were included in this analysis. The mean age was 56.9 ± 14.8 years, 63% were male. Pre-operative TTEs occurred at a median of 215 (IQR 105-390) days before transplant. Baseline demographics are presented in Table 1.
Survival analysis was performed after adjusting for age, sex, diabetes, hypertension, and delayed graft function, using Cox regression model. A total of 205 patients (58%) normalized their RVSP following surgery. Patients who had improvement of RVSP to ≤ 40mmHg, “reversible” PHTN, post-transplant had significantly improved survival at five years compared to those with “persistent” PHTN (88.3% vs 73.3%, p<0.001) (Figure 1).
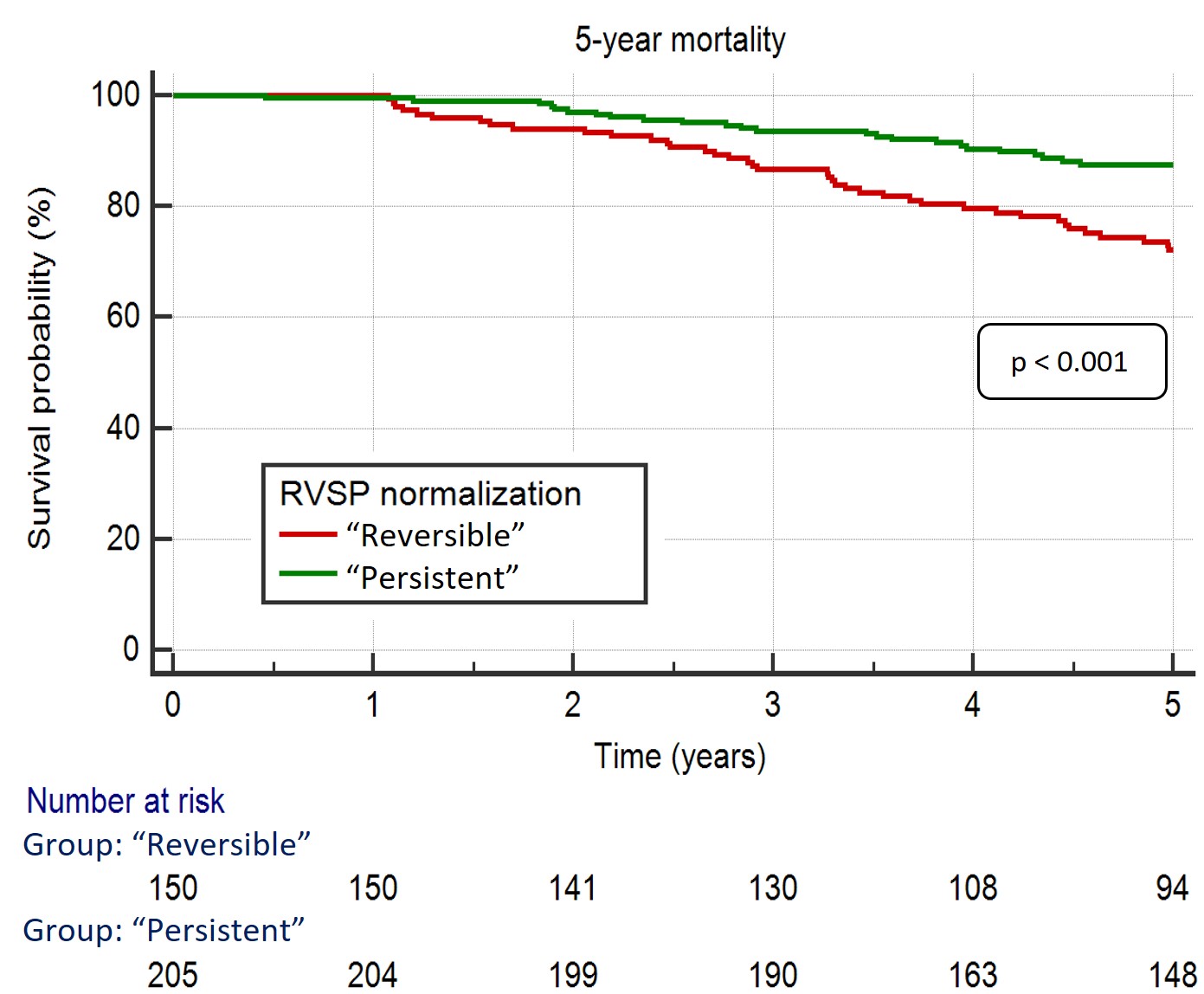
Conclusions: Normalization of PHTN after transplant was not uncommon and resulted in significant survival benefit at five years post-transplant. This study highlights that pre-transplant PHTN may not be always fluid related, and persistence of the same post transplant may lead to adverse outcomes.
[1] Transplant outcomes
[2] Pulmonary hypertension
[3] Echocardiography
