Kidney transplantation in patients with Multiple Myeloma (MM) and Monoclonal Gammopathy of Renal Significance (MGRS)
Sonja Gracin1,2, Marie Felldin1,2, Cecilie Hveding Blimark2,3.
1Transplant Centre, Sahlgrenska University Hospital, Gothenburg, Sweden; 2Gothenbug University, Division of Medicine, Gothenburg, Sweden; 3Department of Haematology and Coagulation, Sahlgrenska University Hospital, Gothenburg, Sweden
Introduction: This is an exciting and new chapter in transplant medicine, ever since the International Kidney and Myeloma Group (IKMG) first recognized the need to identify and classify MGRS. Still, there is very limited knowledge of the prevalence of MGRS in the Nordic countries and wider, and treatment experience worldwide is lacking. There is not a unified pathology diagnosis in MGRS and very limited real world data data in national registers (or none in case of MGRS in Sweden) on the treatment with kidney -tx. The situation with MM is much better, and we have National Myeloma registers in the Nordic countries but limited treatment data regarding kidney transplant. We have observed an increased prevalence of patients with MGRS and MM in haematology clinics in recent years, due to the aging population and novel treatments with better prognosis. Since 1980´s there is a 3-fold increase in prevalence of MM in Sweden. Myeloma survival has improved and as kidney disease is often accompanied in MM, the demand for kidney transplantation is increasing. However, past studies, mainly from Mayo Clinic in Rochester, showed that the risk for disease recurrence in MGRS in very high, especially early after kidney transplantation and often the cause for graft loss and death. This is the main motive for further research and active collaboration.
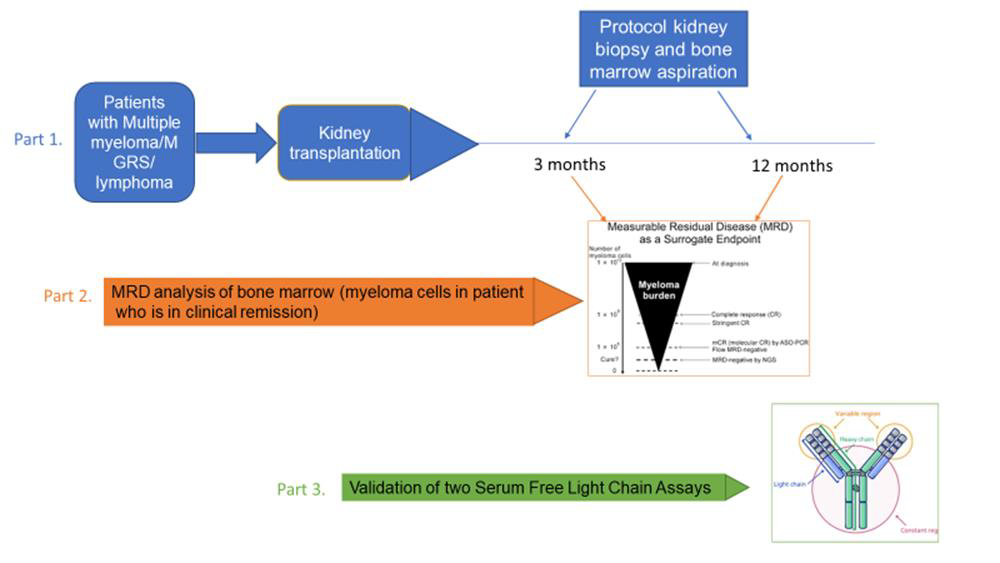
Methods and Results: In order to improve prognosis after kidney transplantation, we have formed an MGRS expert group at Sahlgrenska University Hospital in Gothenburg and created a kidney transplant protocol proposal in MM and MGRS patients. It includes pretransplant treatment, remission assessment, posttransplant maintenance therapy and surveillance with protocol kidney biopsies and protocol bone marrow punction with novel diagnostic tool MRD (minimal residual disease) after kidney transplantation. During our work we´ve recognised the need to extend the collaboration and offer it to experts in Nordic countries, which led into forming of two expert groups: Haematology and Nephrology Expert Group in MM/MGRS and kidney transplant with experts from Sweden Norway Finland and Denmark This work is ongoing, with plan to start implementing the protocol in next months.
Conclusion: Kidney transplantation in MGRS and MM is a challenging topic. By introducing the new diagnostic and treatment protocol, we hope to be successful in detecting early and subclinical recurrence of the primary disease after kidney transplantation, in collaboration with Norway, Denmark and Finland and achieve better results, gather experience and develop further research. We look forward to present our first data on one of our next meetings.
[1] Kidney transplantation
[2] Monoclonal Gammopathy of Renal Significance (MGRS)
[3] Multiple Myeloma (MM)
