Relationship between pre-transplant and post-transplant echocardiographically derived left atrial volume index and clinical outcomes in kidney transplant recipients
Isabel Scalia1,2, Juan M. Farina1, Chadi Ayoub1, Samy Riad2, Hani Wadei2, Lisa Lemond1, Reza Arsanjani1, Girish K. Mour1.
1Division of Cardiovascular Diseases, Mayo Clinic, Phoenix, AZ, United States; 2Division of Internal Medicine, Nephrology, Mayo Clinic, Phoenix, AZ, United States
Introduction: Elevated left atrial volume index (LAVI) on transthoracic echocardiography (TTE) is known to be independently associated with atrial fibrillation (AF) and all-cause mortality in both the general population and in patients with end stage renal failure, however the impact of renal transplant on LAVI and consequent clinical outcomes has not yet been evaluated. The primary clinical outcome was all-cause mortality based on pre transplant elevated LAVI vs normal LAVI. We, further, did a sub group analysis in the elevated LAVI cohort to assess new diagnosis of AF post-transplant and mortality based on post LAVI measurements.
Methods: Retrospective review was conducted for all consecutive patients who underwent solitary kidney transplantation across three academic centers between 1/1/2011 and 09/30/2021. LAVI was collected from the most recent TTE prior to renal transplant as well as the first TTE after six months post-transplant. Diagnosis of AF prior to transplant as well as baseline comorbidities were abstracted from electronic medical records. The cohort was divided based on pre-transplant LAVI; normal (≤ 35 mL/m2) or abnormal (> 35 mL/m2). Patients with pre-operative abnormal LAVI were then assessed for changes in LAVI post-transplant and recognized as “normalizer” (post-transplant LAVI ≤ 35 mL/m2) and “non-normalizer” (post-transplant LAVI > 35 mL/m2).
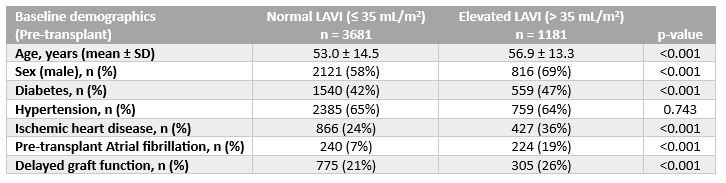
Results: A total of 4862 patients were reviewed. Baseline characteristics are presented in Table 1.
Survival analysis after adjusting with Cox regression for age, sex, diabetes, hypertension, and delayed graft function revealed significantly higher mortality at five years for patients with elevated pre-transplant LAVI compared to normal LAVI (17% vs 12%, p < 0.001) (Figure 1A).
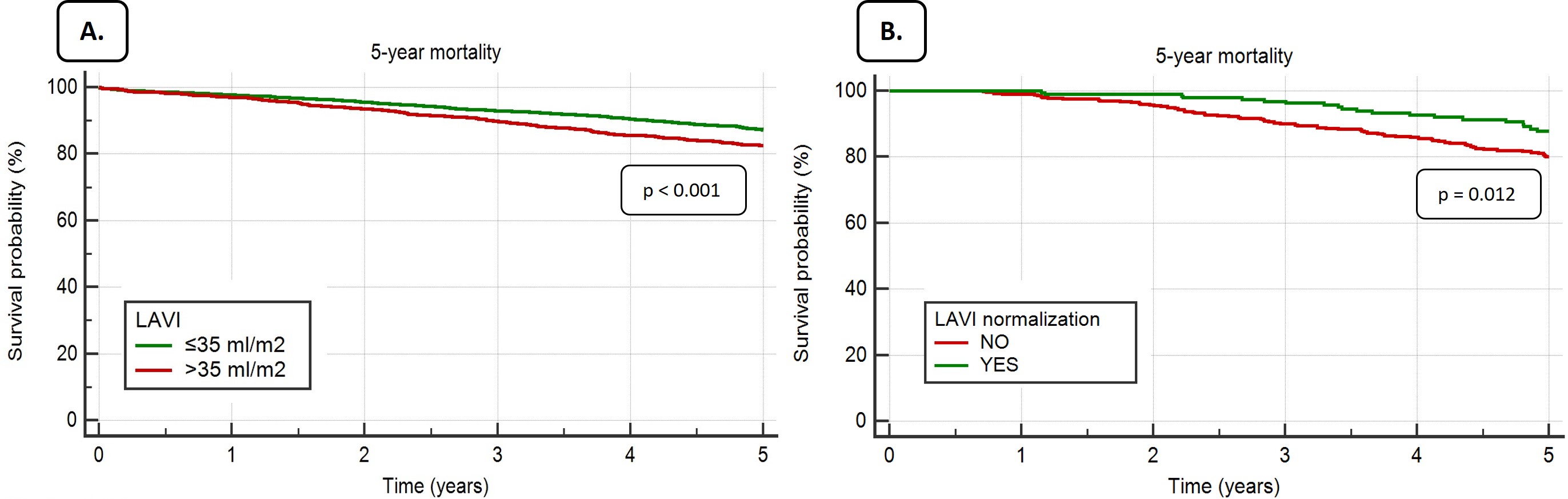
Among 587 cases with abnormal pre-operative LAVI who underwent post-transplant TTE, 189 (32%) normalized their left atrial volume. In “non-normalizers”, mortality was significantly higher compared to those who had a substantial improvement of LAVI post-transplant (“normalizers”) (20% vs 11%, p = 0.012) (Figure 1B). “Normalizers” also had a lower incidence of new AF post-transplant compared to “Non-normalizers” (26% vs 50%, p<0.001).
Conclusions: Elevated LAVI pre-transplant is independently associated with significant mortality in renal transplant recipients. Importantly, normalization of LAVI confers both a survival benefit as well as a reduction in risk of AF at five years post-transplant. These findings reveal the clinical significance of pre-operative LAVI assessment and potential avenue for interventions to mitigate morbidity and mortality post-transplant.
[1] Kidney transplant
[2] Echocardiography
[3] Left atrial volume index
