
Health-related quality of life after living kidney donation by group comparison: a systematic review and meta-analysis
Stijn Laar1,3, Hidde de Heus1, Emma Massey2, Robert Porte1, Frank Dor3, Robert Minnee1.
1Department of Surgery, Division of HPB & Transplant surgery, Erasmus Medical Center Transplant Institute, University Medical Center Rotterdam, Rotterdam, Netherlands; 2Department of Internal Medicine, Division of Nephrology, Erasmus Medical Center Transplant Institute, University Medical Center Rotterdam, Rotterdam, Netherlands; 3Imperial College Renal and Transplant Centre, Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, United Kingdom
Living donor kidney transplantation (LDKT) is recognized as the most effective treatment for end-stage kidney disease, offering superior outcomes compared to deceased donor kidney transplantation or dialysis. The assessment of health-related quality of life (HRQoL) following living kidney donation (LKD) is crucial given that a healthy individual willingly undergoes the procedure. This meta-analysis aims to present the most recent evidence on HRQoL after LKD since LDKT rates are increasing yearly. However, there is conflicting evidence regarding the post-donation quality of life. Our hypothesis posits that the HRQoL of donors after LKD is comparable to pre-donation levels and other relevant populations, including potential living kidney donors, the general population, and healthy controls.
To achieve this objective, comprehensive searches were conducted up to December 11th, 2023. Our primary outcome measures included the SF-36 and composited mental- (MCS) and physical component scales (PCS), comparing post-donation HRQoL to baseline or the general population.
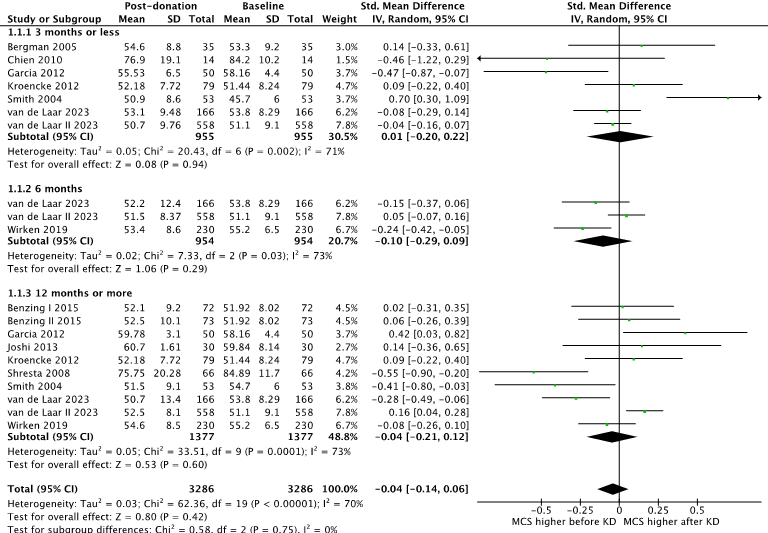
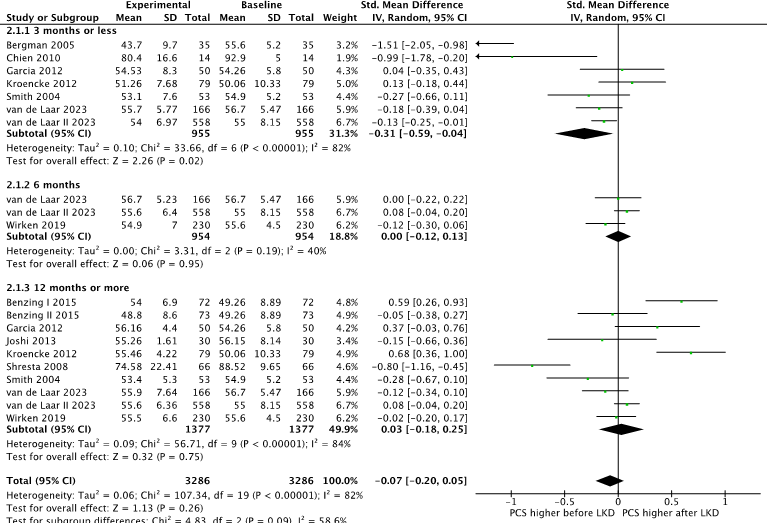
A total of 70 studies encompassing 15,666 patients were included in this meta-analysis. The MCS did not show a significant difference at 3, 6, and 12 or more months post-transplantation compared to baseline (Figure 1), with an overall standard mean difference (SMD) of -0.04 (95% CI: -0.14 to 0.06, p = 0.75). However, the PCS demonstrated a significantly lower HRQoL at 3 months (Figure 2), with an SMD of -0.31 (95% CI: -0.59 to -0.04, p = 0.02). Nonetheless, no significant differences were observed at 6 and 12 months post-transplantation, with an overall SMD of -0.07 (95% CI: -0.20 to 0.05, p = 0.09).
Both PCS and MCS were significantly higher compared to the general population. Furthermore, the separate domains of SF-36 were significantly decreased at 3 months post-transplantation. However, these domains were significantly increased at 12 months post-transplantation, with an SMD of 0.63 (95% CI: 0.60 to 0.66, p < 0.001). Compared to the general population, SF-36 domains were significantly higher at 3, 6, and 12 months or more post-transplantation. There was no difference when comparing the living kidney donors to healthy controls, potential living donors and better compared to dialysis patients. When comparing between different groups of living donors, we found that younger donors had significantly better general health and physical functioning compared to older donors and there was no difference between male or female living donors, amongst others.
Based on the available evidence, HRQoL appears to be diminished shortly after living donor kidney donation but does not exhibit a significant difference or significantly higher levels after a year or longer post-donation. Furthermore, living donors have significantly higher HRQoL compared to the general population. These findings suggest that HRQoL should not serve as a deterrent for living kidney donation.
[1] Living donor kidney transplantation
[2] Health-related quality of life
[3] Mental health
