The relationship between the presence and severity of preoperative metabolic associated fatty liver disease and the development of postoperative diabetes mellitus in renal transplant patients
Ece Gul Kose Hamidi1, Deniz Turkum Atikcan Simsek1, Mustafa Senturk2, Ozlem Turhan Iyidir1, Aslı Nar1, Afig Gojayev3, Sedat Yildirim3, Neslihan Bascil Tutuncu1, Mehmet Haberal3.
1Endocrinology and metabolism, Baskent University, Faculty of Medicine , Ankara, Turkey; 2Internal medicine, Baskent University, Faculty of Medicine , Ankara, Turkey; 3General surgery, Baskent University, Faculty of Medicine , Ankara, Turkey
Renal transplantation.
Introduction: Metabolic associated fatty liver disease (MAFLD); is a range of conditions characterized by the presence of hepatic steatosis and the absence of secondary causes of hepatic steatosis, such as alcohol consumption, chronic use of medications that can cause hepatic steatosis, and inherited disorders. While the presence of MAFLD increases the risk of type 2 Diabates Mellitus (DM) development and DM-related complications; the presence of type 2 DM also increases the severity of MAFLD and the incidence of MAFLD-related complications. In transplant patients as well as in the normal population, the sonographic presence of MAFLD before transplantation is associated with the development of new-onset diabetes and significant metabolic consequences. Our aim in this study was to evaluate the relationship between the presence and severity of preoperative MAFLD and the development of postoperative DM in patients who underwent renal transplantation in our center.
Method: Data on patients who underwent renal transplantation in our hospital between 2000 and 2023 were analyzed retrospectively. Preoperative abdominal ultrasonography and pre/postoperative FIB-4 score (age, AST, ALT, platelet), APRI score (AST, platelet), non-alcoholic fatty liver disease(NAFLD) fibrosis score (age, Body mass index, AST/ALT ratio, platelet, albumin, impaired fasting glucose and the presence of DM), were evaluated, which will be used to determine MAFLD severity of the patients.
Results: The data of 351 patients included in the study are shown in Table 1.
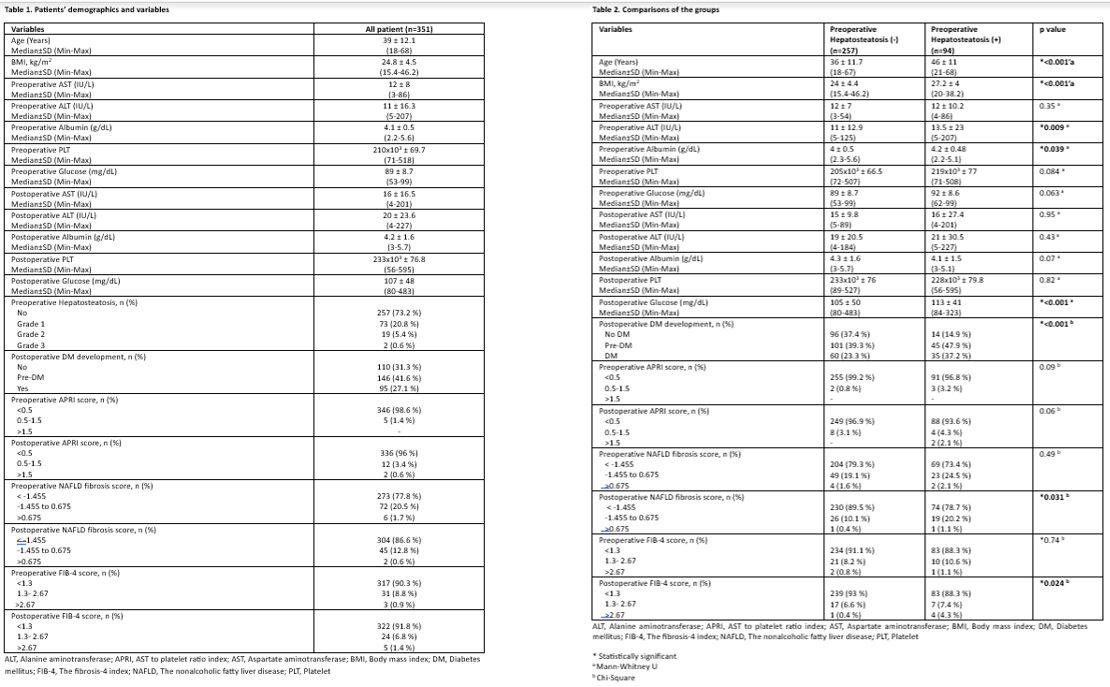
Preoperative hepatosteatosis was not detected in 257 (73.2%) of the patients. Grade 1, grade 2 and grade 3 hepatosteatosis were detected in 73 (20.8%), 19 (5.4%), and 2 (0.6%) patients, respectively. DM and pre-DM developed in postoperative period in 95 (27.1%) and 146 (41.6%) patients, respectively. When patients were divided into two groups according to the presence of hepatosteatosis; age (p<0.001), body mass index (p<0.001), preoperative ALT (p=0.009), postoperative glucose (p<0.001), postoperative DM development rate (p<0.001), postoperative NAFLD fibrosis score (p=0.031) and postoperative FIB-4 (p=0.024) score were statistically significantly higher in the group with hepatosteatosis. However, preoperative albumin (p=0.039) was statistically significantly lower in the group with hepatosteatosis. All comparisons are shown in table 2. The patients also were divided into 3 subgroups according to DM development status in the postoperative period. Compared with other groups, the preoperative FIB-4 score (83.2% vs. 98.2% and 89%, p=0.005), postoperative FIB-4 score (85.3% vs. 98.2% and 91.1%, p=0.018) and NAFLD fibrosis score (75.8% vs. 92.7% and 89%, p=0.007) of patients who did not develop DM were significantly lower than other subgroups (Table 3).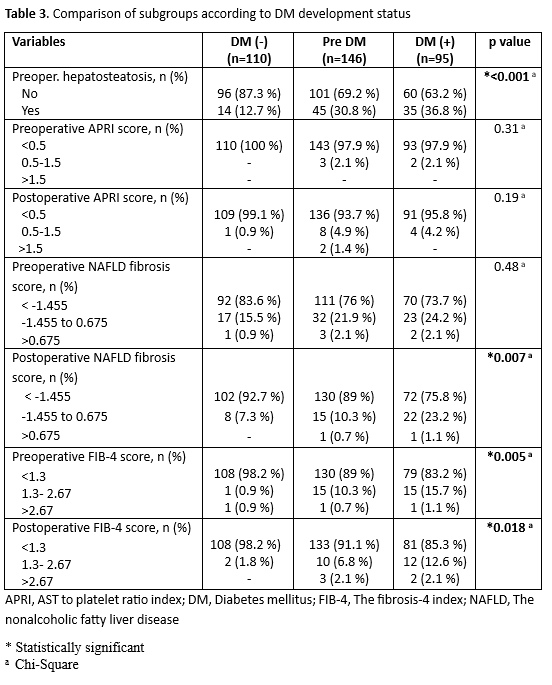 .
.
Conclusion: Preoperative sonographic evaluation of presence and severity of MAFLD in patients whom planned for renal transplantation are very important to predict the development of postoperative DM.
[1] renal transplantation, hepatosteatosis, diabetes mellitus
